Kidneys Aren’t Harmed When Significantly Lowering Blood Pressure
Published Date
Article Content
Using a novel biomarker panel to track and measure kidney function, researchers at University of California San Diego School of Medicine and University of California San Francisco School of Medicine report that lowering systolic blood pressure to less than 120 mm Hg does not damage the kidney organ itself. Instead, any negative changes to clinical results are more likely due to decreased blood flow.
Previously, physicians believed significantly lowering high blood pressure in hypertensive patients damaged the kidneys.
The findings are published in the October 23 issue of Annals of Internal Medicine.
“There has always been debate surrounding how aggressively blood pressure should be treated since more aggressive treatment would require more medications and strain on the kidneys,” said Joachim H. Ix, MD, chief of the Division of Nephrology-Hypertension at UC San Diego School of Medicine. “However, we now have evidence that apparent changes in kidney function are predominantly the result of less blood flood, not damage.”
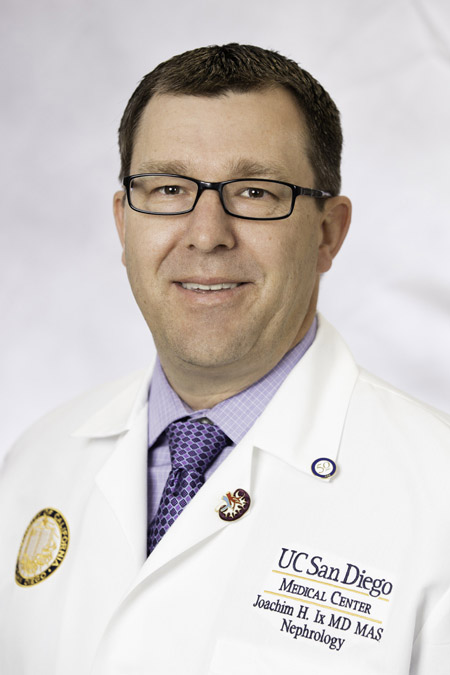
Joachim H. Ix, MD, chief of the Division of Nephrology-Hypertension at UC San Diego School of Medicine.
“The available tests that clinicians typically use to monitor kidney health are both antiquated and inadequate. The creatinine test results are leading clinicians to make the wrong decisions around blood pressure treatment,” said Michael G. Shlipak, MD, MPH, scientific director of the Kidney Health Research Collaborative at UC San Francisco School of Medicine. “There is an urgent need to bring new kidney tests into clinical practice, so that we can monitor the health inside the kidney.”
The Systolic Blood Pressure Innovation Trial (SPRINT) was a large clinical trial that randomized hypertensive individuals to receive intensive blood pressure lowering to less than 120 versus standard of care. Using a subset of data from SPRINT, researchers designed a nested case-control study with 162 participants who did not develop chronic kidney disease (CKD). These patients were matched to SPRINT participants who had been diagnosed with incident CKD based on changes in serum creatinine — the main clinical marker of kidney function — during the course of the trial. By comparing nine urinary biomarkers that are known to mark intrinsic kidney damage, researchers were able to compare measurements between these groups at baseline and one-year of follow-up.
“More intensive blood pressure lowering to a target of 120 saves lives and prevents cardiovascular events, but this was previously counter-balanced by perceived risks of kidney,” said Ix. “The mortality and cardiovascular disease benefits are major reasons to consider being more aggressive with your blood pressure management. The new data suggest that this can be accomplished without any real damage to the kidneys.”
Hypertension affects more than 100 million American adults. Uncontrolled over time, high blood pressure can cause narrowing of the arteries and slow or block blood flow to the kidneys. This can cause CKD. If untreated, CKD can lead to kidney failure.
Ix said his team would like to conduct studies with longer follow-up, and extend their investigation to other conditions where treatments may cause blood flow changes to the kidney, but may not necessarily cause kidney damage.
“We are excited to use the new biomarker panel on future studies to further define the differences in intrinsic kidney damage verses changes from a reduction in blood flow,” said Ix. “With close to 10 percent of Americans suffering from kidney disease, these future research studies could have a large impact.”
Co-authors include: William R. Zhang, BS, Kidney Health Research Collaborative, Veterans Affairs Medical Center, San Francisco, CA; Timothy E. Craven, MSPH, Wake Forrest School of Medicine; Rakesh Malhotra, MD, UC San Diego; Mark J. Sarnak, MD, Tufts University; Alfred K. Cheung, MD, University of Utah; Michel Chonchol, MD, University of Colorado; Paul Drawz, MD, University of Minnesota; and Chirag R. Parikh, MD, Yale University. All from the SPRINT Research Group.
Funding for this research came, in part, from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK098234).
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.