Muscle as a Heart-Health Predictor
Men with greater abdominal muscle area show an increased risk of coronary heart disease
Story by:
Media contact:
Published Date
Story by:
Media contact:
Topics covered:
Share This:
Article Content
Body composition — often expressed as the amount of fat in relation to muscle — is one of the standard predictors of cardiac health. Now, new research from the University of California San Diego Herbert Wertheim School of Public Health and Human Longevity Science indicates more muscle doesn’t automatically mean lower risk of heart trouble.
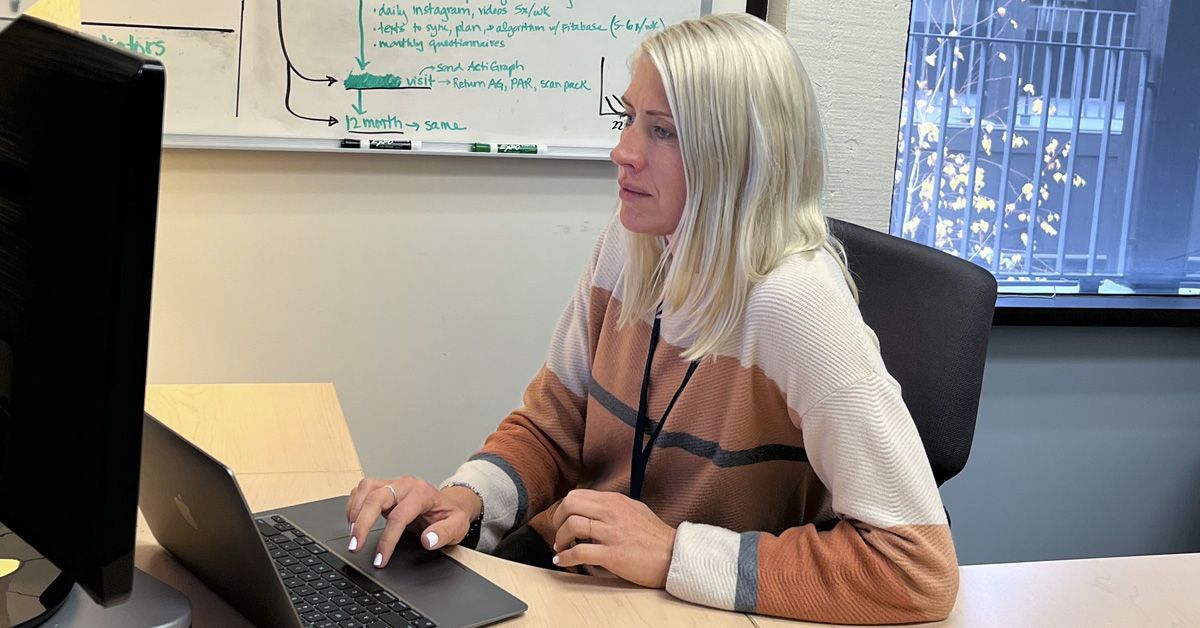
The study, published in the Journal of the American Heart Association, found all muscle isn’t the same. Britta Larsen, PhD, says men with a higher area of abdominal muscle have a greater risk of cardiac trouble. It’s a completely different story for men with greater muscle density. The denser the muscle, the better: Men with the densest muscle in their abdominal cavity had about one quarter the risk of coronary heart disease later on.
“And the other really important thing to note is that we didn't find this with women. It was just in men,” said Larsen, lead author and associate professor in the UC San Diego Herbert Wertheim School of Public Health and Human Longevity Science.
The data were taken from computed tomography of subjects in the National Institutes of Health Multi-Ethnic Study of Atherosclerosis, or MESA. Larsen explained that the subjects were in their mid-60s when the study — aimed at the understanding of the thickening of the arteries — began in the year 2000. Participants were recruited from numerous places around the U.S. and had follow-up visits for 20 years. Larsen noted that her group followed the subjects’ medical records for 12 years.
The researchers found that the large-muscle group’s heart-disease risk was as much as six times higher than the group of men with the smallest abdominal muscle area. Larsen said the team was surprised by the correlation of higher muscle area with higher coronary heart disease.
“Muscle has been overlooked in health for a long time,” Larsen said. “Researchers have really just focused on fat. But muscle is a large, active metabolic tissue, and it's finally getting a little bit more attention.”
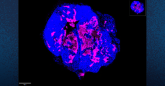
Larsen explains the distinction between muscle area and muscle density boils down to quantity vs quality. The computed tomography scans render a two-dimensional image. Muscle area, she said, was determined simply by pixel count in the image.
“Density is a little bit trickier. It's sort of our proxy measure of muscle quality,” Larsen said. “It's really a measure of how much fat has infiltrated the muscle cavity. Within the muscle itself, how much is pure muscle? And how much is fat content?”
The study also found no correlation between muscle and stroke, among men as well as women. The researchers drew a distinction between coronary heart disease and cardiovascular disease, which includes stroke — a block in the artery outside the heart.
“What that tells me is that muscle density isn't just sort of a proxy measure of overall health or frailty or aging,” she said. “Otherwise, we would see it with stroke and other outcomes, too.”
Larsen said the work raises many more questions and possible avenues for future research. For instance: Why are women seemingly exempt from the muscle/coronary connection?
Larsen said a larger question concerns the biological mechanisms driving the muscle/coronary connection in men. Genetics could be involved, but she said her suspicions turn to diet and physical activity.
Larsen’s collaborators on the work and co-authors on the paper from Herbert Wertheim School of Public Health and Human Longevity Science include John Bellettiere, Rowena M. Tam and Rita Ryu. Other collaborators are Matthew Allison, Michael Criqui and Jonathan Unkart, all of the Department of Family Medicine at UC San Diego; Robyn L. McClelland, Department of Biostatistics, University of Washington; Iva Miljkovic, Department of Epidemiology, University of Pittsburgh; Chantal Vella, Department of Movement Sciences, University of Idaho; and Pamela Ouyang, Department of Medicine, Johns Hopkins School of Medicine.
“Muscle has been overlooked in health for a long time. Researchers have really just focused on fat. But muscle is a large, active metabolic tissue, and it's finally getting a little bit more attention.”
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.