UC San Diego and Scripps Research Join National Team to Make Vision-restoring Whole Eye Transplants a Reality
Technologies developed by both teams will map the human eye-brain connectome, extend the lifespan of the revived human eye, and help regenerate and monitor the optic nerve after a whole eye transplant
Story by:
Published Date
Article Content
A San Diego team is part of a major undertaking that will bring together more than 40 scientists, doctors, and industry experts hand-picked from around the country to make vision-restoring whole eye transplants a reality.
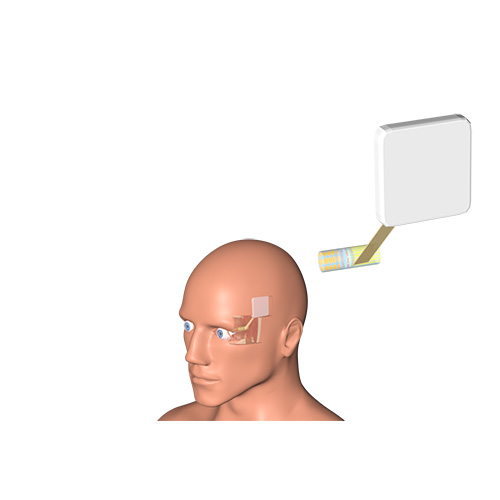
At UC San Diego, a research team led by Professor Shadi Dayeh, in the Department of Electrical and Computer Engineering, will develop a wireless, multi-modal electrode system to wire the optic nerve to the brain with high-end precision after an eye transplant to restore vision.
At Scripps Research, a research team led by Associate Professor Anne Hanneken, in the Department of Molecular Medicine, will advance neuroprotective surgical protocols, perfusion techniques and monitoring systems to support the long-term viability of the whole eyes and the surgical transplant procedure.
The groundwork for this UC San Diego-Scripps Research collaboration began several years ago when Dr. Hanneken and Professor Dayeh were introduced by Ian Galton, a professor of electrical engineering at UC San Diego and former patient of Dr. Hanneken. Early brainstorming sessions between the three scientists focused on the possibility of directing and inducing optic nerve regeneration in the revived human eye using electrical stimulation.
Dr. Hanneken, who is a pioneer in donor human eye revival, and Professor Dayeh, who will serve as the neuromodulation architect on the project, will jointly work with Dr. Jeffrey Goldberg, Blumenkranz Smead professor and chair of ophthalmology at the Byers Eye Institute at Stanford University, the principal investigator for the project. Dr. José-Alain Sahel, professor and chair of the Department of Ophthalmology at the University of Pittsburgh, will co-direct the initiative with Goldberg.
Credit: Jungho Yi of the Dayeh’s lab at UC San Diego
“This breakthrough electrode interface technology together with the end-to-end systems we developed here at UC San Diego will map the human eye, optic nerve, and visual cortex at unprecedented resolution, and help regenerate the optic nerve after an eye transplant,” Dayeh says. “Together with Anne Hanneken and our partners across the nation, we embark on an extraordinary opportunity to transform vision science and to tackle blindness and advanced visual degeneration.”
“The scientific questions we are addressing now are so complicated and complex that you really need the best and brightest collaborators with multidisciplinary expertise to make a true impact,” Hanneken said. “Our recent success in restoring light signaling in postmortem human organ donor eyes was only possible with a great team. This team approach will now allow us to reconsider the prediction made by Dr. Roger Guillemin, Nobel Laureate in Physiology and former president of the Salk Institute, who told me 30 years ago that we would be performing whole eye transplants in my lifetime.”
The award of up to $56 million is from the Advanced Research Projects Agency for Health (ARPA-H) Transplantation of Human Eye Allografts (THEA) program. Led by Stanford University, the awarded project title is Viability, Imaging, Surgical, Immunomodulation, Ocular preservation and Neuroregeneration (VISION) Strategies for Whole Eye Transplant—a reflection of the breadth of the collaboration assembled to solve such a complex challenge.
The biggest challenge the team will face is moving whole eye transplants from aesthetic to functional by figuring out how to regenerate the optic nerve, which connects the eye to the brain.
UC San Diego’s role
Dayeh’s research group invented a biocompatible electrode interface that uses platinum nanorods, known as PtNRs, that can be applied in various areas of the central and peripheral nervous system. The devices come in various forms, including electrode arrays with thousands of channels to capture brain activity in unprecedented resolution. Dayeh, whose research was funded by NSF and the NIH Director’s New Innovator Award, is the principal investigator on an NIH-funded BRAIN Initiative project involving multiple institutions that is using the technology to develop a wireless epilepsy monitoring system. The Federal Drug Administration recently approved a clinical trial to test the effectiveness of an electronic grid developed by Dayeh’s team to record brain activity during surgery.
In the early phases of the THEA-VISION project, Dayeh and colleagues aim to use a grid composed of tens of thousands of light emitting diodes to stimulate the retina and map topographical organization of the retinal-optic nerve-brain pathways in animals and in humans. In later phases, Dayeh’s group will use human-grade, inflatable electrodes they developed to stimulate and help regenerate the optic nerve. The electrodes can generate electrical signals, which would help direct the growth of the axons inside the optic nerve to re-establish connection between the transplanted nerve and the brain.
Partners at UC San Diego are professors Ian Galton, Hanh-Phuc Le and Drew Hall, all in the Department of Electrical and Computer Engineering, as well as Dr. David Roth in the Department of Anesthesiology, and Karen Tonsfeldt, a project scientist in biological sciences and electrical engineering. Dayeh will also collaborate with Drs. Hoi Sang U and Marc Schwartz of the Department of Neurological Surgery, and Dr. Derek Welsbie in the Department of Ophthalmology.
Dayeh’s Integrated Electronics and Biointerfaces Laboratory (IEBL) team, composed of postdoctoral scholars Jungho Yi, Hyeonseok Kim, Wonjae Jeon, Keundong Lee, Jihwan Lee, and Ritwik Vatsyayan, graduate students Kaushik Shukla, Kevin Coffey, Shawn Fisher, Tianhai Wu, Tara Porter, Hao Le, Andrew Bourhis, Jing Gu, and Fadi Khoury, and residents Drs. Kiefer Forseth and Mickey Abraham from the Department of Neurological Surgery, Dr. Bernd Fruhberger, the IEBL GMP lab director, and Nauleen Khan, the IEBL quality quality assurance specialist, will focus on translational animal and human experiments.
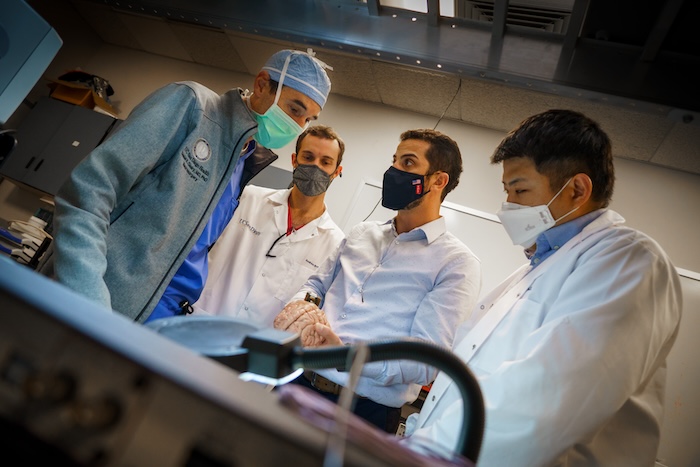
Photo: David Baillot/UC San Diego Jacobs School of Engineering
Scripps Research’s role
Hanneken is a vitreoretinal surgeon and an innovator in the field of human organ donor eye revival. She organized a multidisciplinary team of vision scientists who collaboratively developed the surgical protocols and techniques that led to the revival of light signaling and trans-synaptic communication in the retina from postmortem organ donor eyes—in other words, they were able to ‘awaken’ the retinal cells and promote communication between them even after death. Published in the journal Nature in 2022, this research opened the doors for feasibility studies in whole-eye transplantation. Funding for this high-risk, high-reward research was provided by grateful patients and philanthropic sources seeking to support a highly transformative program. Additional funding is now provided by the National Eye Institute.
During the THEA-VISION project, the Hanneken lab will support a multitude of highly collaborative projects focused on preclinical, clinical and discovery phases of the study. The primary aim is to identify strategies for optimizing the viability and long-term survival of the organ donor eyes and maximize their function following transplantation and optic nerve regeneration. Ocular perfusion prototypes will be designed to provide oxygenation and metabolic support to the whole eye. Automated, physiologic sensors will also be integrated into these perfusion devices to maximize the eyes’ survival. Mapping the topographical organization of the retinal-optic nerve-brain pathway–understanding the intricacies of how the brain and eye are connected–will be performed by connecting the grids containing the light-emitting electrodes to the retina while the neurosurgical team measures the electrical signals in the optic nerve and brain.
In addition to partnering with the Dayeh team at UC San Diego, the Hanneken laboratory will team with vision scientists, physicians and medical personnel at the Salk Institute, University of California - Los Angeles, Cedar Sinai Medical Center, LifeSharing, One Legacy, the San Diego Eye Bank, Scripps Memorial Hospital and Scripps Clinic.
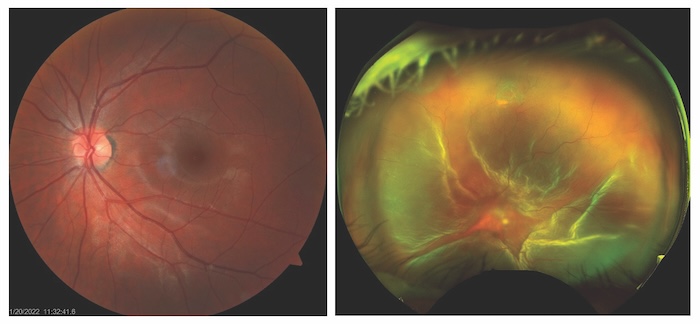
Credit: Scripps Research
The ‘whole’ plan
The VISION for Whole Eye Transplant project is holistic in every sense of the word.
The team is made up of a potent mix of expertise and skill, which will be needed as they simultaneously advance and create cutting-edge medical devices, artificial intelligence integrations, new surgical techniques, regenerative medicine breakthroughs and rejection mitigation. The group will work dynamically, sharing information in real-time and pursuing the most promising leads.
Meticulous donor eye selection, advanced ocular imaging and specialized logistics in organ procurement and preservation will also be critical for success, and collaborators on this team are already the established leaders in these key areas of transplant science. In the end, tailored post-care rehabilitation for eye recipients will also be needed to set patients on the right track.
Amid the technical details, accessibility plays a major role in the plan.
While whole eye transplants are the north star of the three-phase, six-year project, the effort will undoubtedly bring with it more breakthroughs along the way, and that is just as exciting, researchers said.
This research was, in part, funded by the Advanced Research Projects Agency for Health (ARPA-H). The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the United States Government.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



