T Cells Can Activate Themselves to Fight Tumors
UC San Diego scientists find an auto-signaling mechanism driving the T cell anti-tumor response
Published Date
Story by:
Media contact:
Topics covered:
Share This:
Article Content
When you need a bit of motivation, it often has to come from within. New research suggests cancer-fighting immune cells have found a way to do just that.
Scientists at University of California San Diego have discovered a property of T cells that could inspire new anti-tumor therapeutics. Through a previously undescribed form of cell auto-signaling, T cells were shown to activate themselves in peripheral tissues, fueling their ability to attack tumors.
The study, published May 8, 2023 in Immunity, was led by study first author and postdoctoral fellow Yunlong Zhao, PhD, and co-senior authors Enfu Hui, PhD, professor in the School of Biological Sciences at UC San Diego and Jack D. Bui, MD, PhD, professor of pathology at UC San Diego School of Medicine.
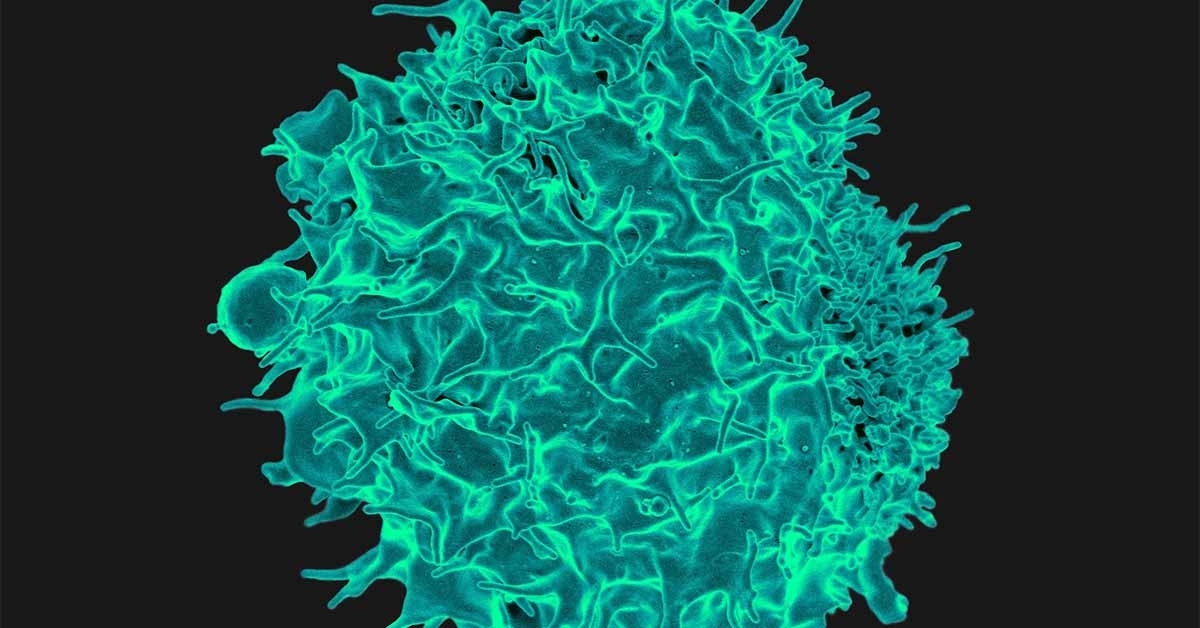
T cells are a type of white blood cell that protect against infection and help fight cancer. In the lymph organs, T cells are trained by antigen-presenting cells, which, as their name suggests, present an antigen (a piece of tumor or pathogen) to T cells, stimulating an immune response.
A key part of this process is the binding of B7, a protein on the surface of antigen-presenting cells, with CD28, a receptor on T cells. This B7:CD28 interaction is a major driver of the T cell immune response. Once trained, T cells leave the lymph organs and travel through the body to find and attack their targets.
More recent work has since revealed that T cells can actually produce their own B7 or take the B7 protein from the antigen-presenting cells and bring it along with them, but exactly why they do this has remained unclear. This also led the researchers to wonder whether T cells, now equipped with both a receptor and its ligand, might be able to activate themselves.
Through a series of experiments, the researchers found that T cells could indeed self-activate by puckering their cell membrane inwards to allow the B7 protein and the CD28 receptor to bind to each other.
“People often assume the cell membrane is flat, but it actually looks more like a coastline with lots of coves and bays,” said Hui. “We found that local membrane curvatures are actually a rich dimension of T cell auto-signaling, which is paradigm-shifting in a field that assumed this only happened across cells.”
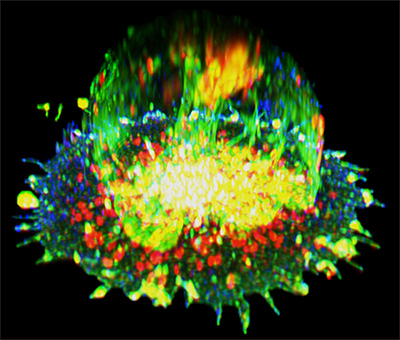
The researchers then confirmed that this auto-stimulation was indeed effective in boosting T cell function and slowing tumor growth in a mouse model of cancer.
“When a T cell exits a lymph organ and enters a tumor environment, it’s like leaving home and going for a long trek in the woods,” said Bui. “The same way a hiker brings snacks to sustain them through the trip, the T cells bring their own signal to keep them going. Now the exciting question is, how much farther will they go if we can provide more food?”
Refueling the T cells could be achieved by either providing more sources of B7 in the lymph organs or in the tumor itself. Another option, the authors say, would be to develop a cell therapy in which engineered T cells with enhanced auto-signaling capabilities were delivered directly to a patient.
The researchers also suggest this system could be used as a cancer biomarker, in that patients whose tumors contain many T cells with B7 may be doing better at fighting the disease.
On the other hand, in patients with autoimmune diseases such as lupus or multiple sclerosis, physicians could prescribe endocytosis inhibitors to prevent the cell from forming concavities, effectively blocking the B7:CD28 interaction to reduce overactive T cell function.
“We’ve found a way that T cells are able to live outside of their normal homes and survive in the foreign environment of a tumor, and we can now develop clinical strategies for increasing or decreasing these pathways to treat disease,” said Hui.
Co-authors include: Yunlong Zhao, Christine Caron, Ya-Yuan Chan, Calvin K. Lee, Xiaozheng Xu, Jibin Zhang and Takeya Masubuchi at UC San Diego, as well as Chuan Wu at the National Cancer Institute.
Funding for this research came, in part, from the National Institutes of Health (grants 1K99AI159295, R37CA239072), the Cancer Research Institute, the Kinship Foundation, The Hartwell Foundation and the Pew Charitable Trusts.
“We’ve found a way that T cells are able to live outside of their normal homes and survive in the foreign environment of a tumor, and we can now develop clinical strategies for increasing or decreasing these pathways to treat disease.”
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.