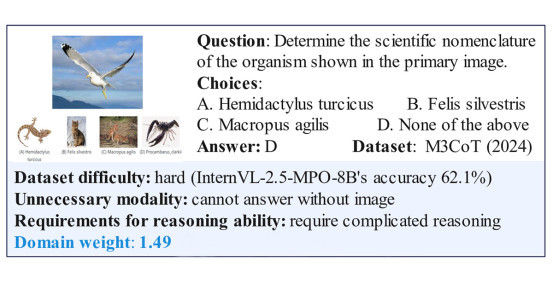
Study: Potential New Treatment Identified for Liver Disease
In a nationwide, multi-center clinical trial, researchers identified a potential new drug that improved liver fibrosis in patients with NASH by 27%
Story by:
Published Date
Story by:
Topics covered:
Share This:
Article Content
Researchers at the University of California San Diego School of Medicine have led a study to examine a potential new treatment option for patients with nonalcoholic steatohepatitis (NASH)-related fibrosis.
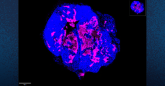
The results, published in the June 24, 2023, online edition of The New England Journal of Medicine, found that a drug that mimics a hormone in the body improved both liver fibrosis, or scarring of the liver, and liver inflammation in patients with NASH.
“Identifying an effective drug for NASH is extremely promising for patients as currently there are no FDA-approved therapies for this condition,” said Rohit Loomba, MD, the study’s first author and chief of the Division of Gastroenterology and Hepatology at UC San Diego School of Medicine. “NASH can adversely impact the quality of life in patients and can progress to cirrhosis. Its complications can lead to death or liver transplantation.”
“Our findings will further the science of this disease and provide a potential new treatment option to those affected by NASH-related fibrosis.”

The researchers found that the drug, called Pegozafermin, mimicked fibroblast growth factor 21 (FGF21) — a liver-secreted peptide hormone that is naturally produced in the body.
FGF21 controls energy use in the body and lipid metabolism in the liver. It has also been shown in previous studies to lower blood glucose and insulin levels, reducing body weight and liver fat.
“The study’s results show that the new potential treatment not only improves fibrosis but also improves inflammation and liver injury along with significant improvements across multiple non-invasive biomarkers of NASH activity and scarring,” said Loomba, gastroenterologist and hepatologist at UC San Diego Health.
The 24-week, randomized clinical trial involved 222 participants with NASH assigned to either receive the drug or a placebo.
Of the patients who received the drug at a higher dose, approximately 27% showed an improvement in liver fibrosis, relative to 7% of the patients who received the placebo. The most frequent reported side effect from the drug were gastrointestinal in nature, including nausea.
Currently, there are no medications approved by the U.S. Food and Drug Administration available for the treatment of NASH, which is a type of nonalcoholic fatty liver disease (NAFLD).
According to the National Institutes of Health, approximately 24% of U.S. adults have NAFLD, and about 6% have NASH.
NAFLD and NASH are considered silent diseases with little to no symptoms; however, individuals who are overweight, have type 2 diabetes or have a family member with NAFLD are at a higher risk of developing the disease. NAFLD — which is an umbrella term for a range of liver conditions affecting people who drink little to no alcohol — can lead to cirrhosis, liver cancer and liver failure.
Loomba adds next steps for this research will be a larger, multi-center, international trial with a more diverse patient population and longer treatment period to better assess the safety of the drug.
“If successfully shown to be both safe and effective in a larger Phase 3 trial, this drug could be used to treat millions of patients with NASH, including our patients at UC San Diego Health,” said Loomba.
Co-authors of the study include: Arun J. Sanyal, MD, Virgina Commonwealth University; Kris V. Kowdley, MD, Washington State University; Deepak L. Bhatt, MD, MPH, Mount Sinai Heart; Naim Alkhouri, MD, Arizona Liver Health; Juan Pablo Frias, MD, Velocity Clinical Research; Pierre Bedossa, MD, PhD, University of Oxford; Stephen A. Harrison, MD, Pinnacle Clinical Research; Donald Lazas, MD, Objective Health; Robert Barish, MD, Ocala GI Research; Mildred D. Gottwald, Pharm.D, Shibao Feng, PhD, Germaine D. Agollah, PhD, Cynthia L. Hartsfield, PhD, Hank Mansbach, MD, Maya Margalit, MD, all at 89bio; and Manal F. Abdelmalek, MD, MPH, Mayo Clinic.
The research was funded, in part, by 89bio, ENLIVEN (Grant Number: NCT04929483) and the National Institute of Diabetes and Digestive and Kidney Diseases (Grant Number: P30DK120515).
Disclosure: Rohit Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Amgen, Anylam/Regeneron, Arrowhead Pharmaceuticals, AstraZeneca, Bristol Myers Squibb, CohBar, Eli Lilly, Galmed Pharmaceuticals, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, Metacrine Inc., NGM Biopharmaceuticals, Novartis, Novo Nordisk, Pfizer, Sagimet, Terns Pharmaceuticals, Theratechnologies, 89 bio and Viking Therapeutics. Research grants were received from Arrowhead Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Gilead, Hanmi Pharmaceutical, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Novo Nordisk, Pfizer, Sonic Incytes, and Terns Pharmaceuticals. Loomba is a cofounder of LipoNexus Inc.
“Our findings will further the science of this disease and provide a potential new treatment option to those affected by NASH-related fibrosis.”
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.