Novel Phage Therapy Saves Patient with Multidrug-Resistant Bacterial Infection
Intravenous viruses are used to target deadly bacterium; dramatic case suggests potential alternative to failing antibiotics
Published Date
Article Content
Scientists and physicians at University of California San Diego School of Medicine, working with colleagues at the U.S. Navy Medical Research Center – Biological Defense Research Directorate (NMRC-BDRD), Texas A&M University, a San Diego-based biotech and elsewhere, have successfully used an experimental therapy involving bacteriophages — viruses that target and consume specific strains of bacteria — to treat a patient near death from a multidrug-resistant bacterium.
The therapeutic approach, which has been submitted to a peer-reviewed journal, is scheduled to be featured in an oral presentation tomorrow at the Centennial Celebration of Bacteriophage Research at the Institute Pasteur in Paris by Biswajit Biswas, MD, one of the case study’s co-authors and chief of the phage division in the Department Genomics and Bioinformatics at NMRC-BDRD. April 27 is Human Phage Therapy Day, designated to mark 100 years of clinical research launched by Felix d’Herelle, a French-Canadian microbiologist at Institute Pasteur who is credited with co-discovering bacteriophages with British bacteriologist Frederick Twort.
Authors say the case study could be another catalyst to developing new remedies to the growing global threat of antimicrobial resistance, which the World Health Organization estimates will kill at least 50 million people per year by 2050. Based on the success of this case, in collaboration with NMRC, UC San Diego is exploring options for a new center to advance research and development of bacteriophage-based therapies.
Robert “Chip” Schooley, MD, professor of medicine and chief of the Division of Infectious Diseases in the UC San Diego School of Medicine.
“When it became clear that every antibiotic had failed, that Tom could die, we sought an emergency investigational new drug application from the FDA to try bacteriophages,” said lead author Robert “Chip” Schooley, MD, professor of medicine, chief of the Division of Infectious Diseases in the UC San Diego School of Medicine and primary physician on the case.
“To our knowledge, he is the first patient in the United States with an overwhelming, systemic infection to be treated with this approach using intravenous bacteriophages. From being in a coma near death, he’s recovered well enough to go back to work. Of course, this is just one patient, one case. We don’t yet fully understand the potential — and limitations — of clinical bacteriophage therapy, but it’s an unprecedented and remarkable story, and given the global health threat of multidrug-resistant organisms, one that we should pursue.”
Infection on vacation

Steffanie Strathdee, PhD, and Tom Patterson, PhD at home.
The story begins in late-2015. Tom Patterson, PhD, a 69-year-old professor in the Department of Psychiatry at UC San Diego School of Medicine, and his wife, Steffanie Strathdee, PhD, chief of the Division of Global Public Health in the Department of Medicine, were spending the Thanksgiving holiday in Egypt when Patterson became ill, wracked by abdominal pain, fever, nausea, vomiting and a racing heartbeat. Local doctors diagnosed pancreatitis — inflammation of the pancreas — but standard treatment didn’t help.
Patterson’s condition worsened and he was medevacked to Frankfurt, Germany Dec. 3, 2015, where doctors discovered a pancreatic pseudocyst, a collection of fluid around the pancreas. The fluid was drained and the contents cultured. Patterson had become infected with a multidrug-resistant strain of Acinetobacter baumannii, an opportunistic and often deadly pathogen. The bacterium has proved particularly problematic in hospital settings and in the Middle East, with many injured veterans and soldiers returning to the U.S. with persistent infections.
Initially, the only antibiotics with any effect proved to be a combination of meropenem, tigecycline and colistin, a drug of last resort because it often causes kidney damage, among other side effects. Patterson’s condition stabilized sufficiently for him to be airlifted Dec. 12, 2015, from Germany to the Intensive Care Unit (ICU) at Thornton Hospital at UC San Diego Health. Upon arrival, it was discovered that his bacterial isolate had become resistant to all of these antibiotics.
At Thornton Hospital, now part of Jacobs Medical Center, Patterson began to recover, moving from the ICU to a regular ward. But the day before scheduled discharge to a long-term acute care facility, an internal drain designed to localize his infection and keep it at bay slipped, spilling bacteria into his abdomen and bloodstream. Patterson immediately experienced septic shock. His heart began racing. He could not breathe. He became feverish and would subsequently fall into a coma that would last for most of the next two months. He was, in effect, dying.
“That’s a period of my life I don’t remember,” recalled Patterson. “There was so much pain that it’s almost beyond your ability to cope. I’m happy not to remember.”
Strathdee, his wife, is no stranger to the terrors of disease. As an infectious disease epidemiologist and director of the UC San Diego Global Health Institute, she has worked around the world, from India to Afghanistan to Mexico, trying to lower HIV infection and mortality rates.
“There came a point when he was getting weaker and weaker, and I didn’t want to lose him. I wasn’t ready to let him go and so I held his hand and said, ‘Honey, they’re doing everything they can and there’s nothing that can kill this bug, so if you want to fight, you need to fight. Do you want me to find some alternative therapies? We can leave no stone unturned.’”
Tom recalled the moment: “I vaguely remember you saying, ‘do you want me to try or not because it’s going to be a tough time and it’s not certain that it will work.’ I remember squeezing your hand, but it was just a flash in the whole process.”
Strathdee began doing research. A colleague mentioned a friend had traveled to Tblisi, Georgia to undergo “phage therapy” for a difficult condition and had been “miraculously cured.” Strathdee had learned of bacteriophages while she was a student, but they were not part of mainstream medical doctrine. She turned to strangers in the phage research community and to her colleague Chip Schooley for help.
Bacteriophages are ubiquitous viruses, found wherever bacteria exist. It’s estimated there are more than 1031 bacteriophages on the planet. That’s ten million trillion trillion, more than every other organism on Earth, including bacteria, combined. Each is evolved to infect a specific bacterial host in order to replicate — without affecting other cells in an organism.
The idea of using them therapeutically is not new. Described a century ago, phage therapy was popular in the 1920s and 1930s to treat multiple types of infections and conditions, but results were inconsistent and lacked scientific validation. The emergence of antibiotics in the 1940s pushed phage therapy aside, except in parts of Eastern Europe and the former Soviet Union, where it remained a topic of active research.
With dwindling options, Strathdee, Schooley and colleagues went looking for help. They found many researchers willing to help. Three teams possessed suitable phages that were active against Patterson’s particular bacterial infection: the Biological Defense Research Directorate of the NMRC in Frederick, MD; the Center for Phage Technology at Texas A&M University; and AmpliPhi, a San Diego-based biotech company specializing in bacteriophage-based therapies. A research team at San Diego State University, headed by microbial ecologist Forest Rowher, PhD, purified the phage samples for clinical use.
With emergency approval from the Food and Drug Administration, each source provided phage strains to UC San Diego doctors to treat Patterson, with no guarantee that any of the strains would actually work. “That’s one of the remarkable things to come out of this whole experience,” said Schooley, “the incredible and rapid collaboration among folks scattered around the world. It was a desperate time and people really stepped up.”
Phage therapy is typically administered topically or orally. In Patterson’s case, the phages were introduced through catheters into his abdominal cavity and intravenously to address a broader, systemic infection, which had not been done in the antibiotic era in the U.S. “That makes them more effective,” said Schooley. “The action is at the interface of the patient and the organism.”
With tweaking and adjustments — his physicians were learning on the fly — Patterson began to improve. He emerged from his coma within three days of the start of IV phage therapy. “Tom woke up, turned to his daughter and said, ‘I love you’,” recalled Schooley. Patterson was soon weaned off of the respirator and blood pressure drugs.
“As a treating doctor, it was a challenge,” said Schooley. “Usually you know what the dosage should be, how often to treat. Improving vital signs is a good way to know that you’re progressing, but when you’re doing it for the first time, you don’t have anything to compare it to.
“A lot was really worked out as we went along, combining previous literature, our own intuition about how these phages would circulate and work and advice from people who had been thinking about this for a long time.”
Treatment details
By the time Patterson was airlifted to Thornton Hospital at UC San Diego Health, he was in dire straits. His abdomen had swelled, distended by the pseudocyst teeming with multi-drug resistant A. baumaunnii. His white blood cell count had soared — a sign of rampant infection.
Doctors tried various combinations of antibiotics. He developed respiratory failure and hypotension that required ventilation and recurrent emergency treatment. He became increasingly delirious. When he lapsed into a coma in mid-January, he was essentially being kept alive on life support. Eventually Schooley said there were no antimicrobial agents left to try. Strathdee recalled colleagues wondering aloud if she was prepared for Tom to die.
She wasn’t. Bacteriophage therapy began March 15, 2016, with a cocktail of four phages provided by Texas A&M and the San Diego-based biotech company AmpliPhi, pumped through catheters into the pseudocyst. If the treatment didn’t kill him, Patterson’s medical team planned to inject the Navy’s phages intravenously, flooding his bloodstream to reach the infection raging throughout his body. As far as Patterson’s doctors knew, such treatment had never been tried before.
On March 17, the Navy phages were injected intravenously. There were fears about endotoxins naturally produced by the phages. No one knew what to expect, but Patterson tolerated the treatment well — indeed there were no adverse side effects — and on March 19, he suddenly awoke and recognized his daughter.
“One of NMRC's goals with respect to bacteriophage science has been providing military members infected with multidrug-resistant organisms additional antimicrobial options so we were experienced and well-positioned to provide an effective phage cocktail for Dr. Patterson,” said Theron Hamilton, PhD, head of Genomics and Bioinformatics at the Navy’s Biological Defense Research Directorate. “Obviously, we are thrilled with the outcome and hope this case increases awareness of the possibility of applying phage therapy to tough cases like this one.”
Subsequent treatment, however, would not be easy. The learning curve was steep and unmarked. There were bouts of sepsis — a life-threatening complication caused by massive infection. Despite improvement, Patterson’s condition remained precarious. Doctors discovered that the bacterium eventually developed resistance to the phages, what Schooley would characterize as “the recurring Darwinian dance,” but the team compensated by continually tweaking treatment with new phage strains — some that the NMRC had derived from sewage — and antibiotics.
In early May, Patterson was taken off of antibiotics. After June 6, there was no evidence of A. baumannii in his body. He was discharged home August 12, 2016.
Post-treatment and beyond
Recovery has not been entirely smooth and steady. There have been setbacks unrelated to the phages. A formerly robust man, Patterson had been fed intravenously for months in the hospital and had lost 100 pounds, much of it muscle. He has required intense physical rehabilitation to regain strength and movement. “It’s not like in the movies where you just wake up from a coma, look around and pop out of bed,” Patterson said. “You discover that your body doesn’t work right anymore.” He said he could feel parts of his brain coming back alive.
Nonetheless, Patterson described the experience as miraculous. Even comatose, when he often wrestled with imagined demons, he recalled hearing and recognizing voices and realizing that beyond his darkness, there was life and hope.
And beyond him, he hopes his experience will translate into new treatments for others: “The phage therapy has really been a miracle for me, and for what it might mean that millions of people who may be cured from multidrug-resistant infections in the future. It’s been sort of a privilege.”
Schooley said Patterson was lucky. His wife was a trained scientist and determined to find a remedy — and they both worked at UC San Diego School of Medicine: “He was fortunate to be in a place that had all of the resources and courage necessary to support him while this innovative therapy was developed, which was essentially a home brew cocktail of viruses to be given to a desperately ill individual. I think a lot of other places would have hesitated. I think the response that he had clinically has been very gratifying and speaks to the strength of a multidimensional medical center with all of the pieces you need.”
Still, Schooley said any broad, future approved application of phage therapy faces fundamental challenges unlike past treatments. “What the FDA is used to saying is ‘This is an antibiotic. We know what its structure is and how you can give it to multiple people.’ With bacteriophage therapy, the FDA would be dealing with an approach in which doctors would have to develop phage cocktails for each patient tailored to their infecting organisms. It’s the ultimate personalized medicine.”
The good news, Schooley said, is that new molecular tools, robotics and other advances make personalized medicine possible in a way it wasn’t 10 or 15 years ago. “Then, it would have been impossible to contemplate. There’s still much research to be done, but I think there are going to be a lot of clinical applications where this approach may be very beneficial to patients.”
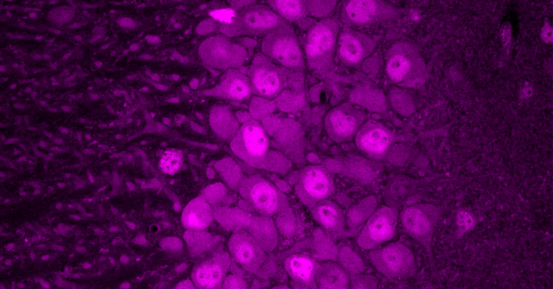
More about bacteriophages
Derived from the Greek words meaning “bacteria eater,” bacteriophages are ancient and abundant — found on land, in water, within any form of life harboring their target. According to Rowher at San Diego State University and colleagues in their book Life in Our Phage World, phages cause a trillion trillion successful infections per second and destroy up to 40 percent of all bacterial cells in the ocean every day.
Thousands of varieties of phage exist, each evolved to infect only one type or a few types of bacteria. Like other viruses, they cannot replicate by themselves, but must commandeer the reproductive machinery of bacteria. To do so, they attach to a bacterium and insert their genetic material. Lytic phages then destroy the cell, splitting it open to release new viral particles to continue the process. As such, phages could be considered the only “drug”’ capable of multiplying; when their job is done, they are excreted by the body.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.