Leading the Way to Health Equity
Researchers across UC San Diego work to understand health disparities—and solve them
Story by:
Published Date
Story by:
Topics covered:
Share This:
Article Content
From developing a 3D virtual human avatar that answers medical questions to mailing at-home colorectal cancer screening tests for individuals from underserved, high-risk groups, researchers from a broad range of fields at the University of California San Diego are making waves as they push the boundaries of science and medicine to develop groundbreaking, real-world solutions to longstanding health inequities.
For certain populations, disadvantage and marginalization, as well as other social determinants, are significant factors in determining an individual’s potential health outcomes. According to the World Health Organization, the most fatal communicable diseases disproportionately affect the world’s poorest populations, and in many cases are compounded by factors such as race, ethnicity, gender, age, sexual orientation or gender identity and migration status.
A pervasive issue of local, national and global concern, health inequity has garnered increased attention in recent years due in large part to disparities highlighted by the COVID-19 pandemic—spurring a renewed sense of urgency to address their underlying causes.
As a world-class public university with a $1.64 billion-dollar research enterprise, UC San Diego promotes a culture of collaboration, experimentation and fresh thinking. Here, interdisciplinary efforts are paramount as researchers leverage their respective areas of expertise to collectively address the world’s most pressing problems. And for those working to understand and address health inequities and disparities, there exists a common goal: to propel society into a future in which all people have a fair chance at reaching optimal health.
“These significant efforts to address health inequities and disparities support our Strategic Plan for Inclusive Excellence. Cultivating a more equitable health system is vital to promoting equal access to health and wellness services for historically underserved groups. It demonstrates our commitment to confronting structural racism in medicine,” said Becky Petitt, Vice Chancellor for Equity, Diversity, and Inclusion. “The lasting impact of this necessary work extends beyond UC San Diego: our researchers are leading the way to establishing a culture of care across the larger healthcare landscape.”
An academic research powerhouse, the university also is home to top-ranked UC San Diego Health, the region’s only academic health system dedicated to clinical, research and teaching excellence. UC San Diego Health and its schools of medicine and pharmacy are committed to promoting health equity as a leader in healthcare access. In fiscal year 2021 alone, UC San Diego Health provided nearly $600 million in uncompensated care, ensuring that all who walk through its doors receive the same leading-edge therapies and world-class patient care.
These efforts are further supported through local initiatives like the UC San Diego Center for Community Health, dedicated to promoting health and wellness in communities with the largest health disparities, and the Student-Run Free Clinic Project at the UC San Diego School of Medicine, an asset to underserved communities in San Diego. To foster a culture of anti-racism throughout its organization, just last year UC San Diego Health recruited Dr. Crystal Cené to serve as its inaugural chief administrative officer for Health Justice, Equity, Diversity and Inclusion.
“Within UC San Diego Health, health equity for our patients is our ‘true north’ metric,” said Cené, who also serves as associate chief medical officer for health equity. “Health equity implies that everyone has a fair and just opportunity to be as healthy as possible. To achieve this, we must value all individuals and populations equally, recognize and rectify historical injustices that created and perpetuate inequities, and provide resources according to need.”
From the Jacobs School of Engineering to the Herbert Wertheim School of Public Health and Human Longevity Science, the School of Global Policy and Strategy and beyond, dozens of experts across UC San Diego’s vibrant campus community are conducting research related to health inequity. The following are just five of many, but their vital work across a wide range of academic disciplines is indicative of a concerted effort—one that positions UC San Diego as a guiding light towards a more equitable future for all.

Developing a virtual human avatar that answers medical questions
People who are isolated, have limited mobility or live in medically underserved communities without ease of access to clinicians often turn to Google or search engines when they have questions about their health conditions, medications, mild symptoms or other health-related topics. But search engines often fail to provide comprehensive medical answers due to the distributed nature of the web. A person might have to visit multiple websites to arrive at a full answer, Ndapa Nakashole, an assistant professor of computer science in the Jacobs School of Engineering at UC San Diego, has found. It can prove time-consuming and overwhelming for a nonexpert to sort through hundreds of pages of search results or comprehend a long and complex answer teeming with medical jargon.
That’s why Nakashole and a collaborative team of UC San Diego researchers and students are working to develop a 3D virtual human avatar—viewable on a computer or mobile app—which answers medical questions by assimilating, synthesizing and storing health information in a broad-coverage resource with a shared vocabulary. In emulating an in-person doctor-patient interaction, the “bot,” which also includes a social mode for companionship, can provide supportive visualizations by highlighting certain parts of the human avatar’s body that are relevant to a particular answer.

This work—which Nakashole plans to expand into other languages that will reach even more underserved communities around the world—has the potential to transform the health of individuals with otherwise limited access to medical care. On the back end, it requires building text generation models that can create fluent, coherent and contextually relevant responses, which is one of Nakashole’s areas of expertise. The research team will also need to develop natural language processing systems—the artificial intelligence models used to train computers to understand spoken and written human language—to translate long, complicated medical questions into versions understandable by the digital avatar.
“If there’s a tool that can aggregate information in providing answers that are comprehensive, that can be really helpful and save people time,” said Nakashole. Her work in artificial intelligence, machine reading and natural language processing first intersected with the healthcare domain four years ago when she and a team of researchers developed a voice assistant, similar to Amazon’s “Alexa” or Apple’s “Siri,” designed specifically to understand and answer the medical questions of older adults—who often are more isolated and tend to have health problems.
In May, Nakashole was awarded a Faculty Early Career Development (CAREER) award by the National Science Foundation to fund the next five years of this work through her project entitled “Informational Extraction and Integration with Applications to Healthcare Question Answering.”
Nakashole and her team are currently working with a medical illustrator to develop the 3D virtual human avatar, and in the future plan to collaborate with robotics experts to create a physical human avatar as an interface for medical question answering. She sees her work as a unique opportunity to make an impact on society and reduce the disparities that are prevalent among certain populations.
“If you can make a difference in people’s lives, that adds much more meaning to the work and makes it that much more worth it,” Nakashole said.
“If you can make a difference in people’s lives, that adds much more meaning to the work and makes it that much more worth it."

Addressing vaccine hesitancy through a pop-up clinic
Since July 2021, more than 90 pop-up clinics have been hosted by Project2VIDA! in the San Diego-Mexico border region, vaccinating approximately 2,000 individuals against COVID-19. The project, aimed at addressing vaccine hesitancy and boosting vaccination rates among Latinx and African American communities in San Diego County, also has linked members of these underserved communities to more than 4,500 total health services ranging from blood pressure and glucose screenings to mental and behavioral health.
It's all part of a team effort spearheaded by Dr. Argentina Servin, Project 2VIDA!’s principal investigator and an assistant professor in the Division of Infectious Disease & Global Public Health at the UC San Diego School of Medicine, who also serves as director of the Bachelor of Science in Public Health program at the Herbert Wertheim School of Public Health and Human Longevity Science.

Servin’s own lived experiences have long shaped her professional career. Growing up without health insurance or proper access to healthcare, she knew at a young age that she wanted to become a doctor and provide care for underserved communities like her own. Now, as a public health researcher, Servin is working to combat the health inequities here in the U.S. that she says were evidenced by the COVID-19 pandemic’s disproportionate effects on certain racial and ethnic groups—including her own Latinx community.
“We tend to have pre-existing conditions, we don’t have access to healthcare, we were always working: the bus drivers, the nurses, the cashier at the grocery store, so we were constantly being exposed. We live in more high-density communities, multi-generational households, so we had other factors that placed us at higher risk,” said Servin, whose family is from Mexico.
In 2020, Servin’s grandfather was hospitalized in an intensive care unit for four months after contracting COVID-19. But even once the vaccine became available, she watched as her family members refused to be vaccinated, largely due to rampant misinformation spreading across the internet. When the National Institute of Minority Health and Health Disparities issued a call for proposals addressing vaccine hesitancy, Servin had an idea: a medical outreach program that would build trust within the local community. She reached out to colleagues both at UC San Diego and San Ysidro Health, and Project2VIDA! was born. Once the team received funding, they began knocking on doors to spread the word about upcoming pop-ups. For Servin, it all comes down to education: opening up conversations about safety standards and the vaccine’s risks and benefits.
“We don’t want to force anyone to get the vaccine,” said Servin, who also has worked with people living with HIV that face barriers to accessing care in the border region. “We come from a very compassionate, non-judgmental approach.”
Her work with Project 2VIDA! goes beyond the vaccine—it’s an opportunity to further understand the barriers that Latinx and African American communities face. Through the pop-ups, Servin and her fellow researchers are collecting data on health disparities and vaccine hesitancy, which may help direct approaches to community healthcare in the future.
More than a year later, Project 2VIDA! continues to host pop-up clinics, where patients now can receive the COVID-19 booster. Servin aims to expand the scope of her research to include parental vaccine hesitancy, particularly when it comes to children 11 and younger. She’s also looking at ways to apply the same framework to other infectious diseases that are preventable through vaccines, like HPV and monkeypox.
“We realized that we have these disparities in care that haven’t been addressed that have been going on for years,” Servin said. “Right now, as we’re transitioning from a pandemic to more of an endemic, I think it’s an important opportunity to rebuild from these lessons learned. Everybody talks about going back to normal—I say we need to get back to a better normal. We can’t go back to the way things were before, because it clearly wasn’t working for everyone.”
"Everybody talks about going back to normal—I say we need to get back to a better normal. We can’t go back to the way things were before, because it clearly wasn’t working for everyone.”
Predicting climate impacts on health in the developing world
Through his work linking weather variation to infectious diseases and nutrition, Gordon McCord, an economist who also is trained in epidemiology, aims to understand how climate change will affect humanity through health—particularly in the developing world, where social determinants like access to food have sizable impacts on population health.

In a study McCord co-authored last year, which explored how the El Niño Southern Oscillation can be used to predict child undernutrition and food insecurity in the developing world, he and fellow researchers emphasized that climate variability is increasingly recognized as a key determinant of health outcomes. Their findings could serve as the basis for early warning systems that could alert aid agencies like Save the Children and the U.N. World Food Programme to which parts of developing nations in Africa, Asia and Latin America will be at highest risk of child malnutrition six months later.
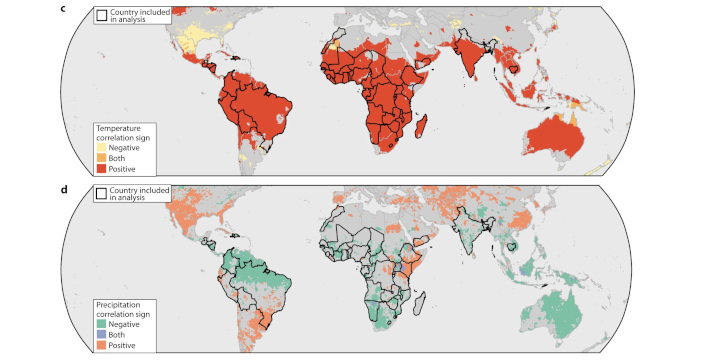
“What that work shows is that when we enter an El Niño, large parts of the world experience weather changes that end up affecting child nutrition,” said McCord, an associate teaching professor of economics and associate dean of student affairs in the School of Global Policy and Strategy at UC San Diego. “When the temperature of the tropical Pacific rises, the world enters an El Niño state. There are some parts of the world that just begin to warm up, and some of those areas have an increase in precipitation while others have a decrease in precipitation, all of which affects agriculture in predictable ways that allow for early warning systems.”
McCord, who also has worked in weather-based modeling for malaria, recently received a grant funded by Wellcome Trust to develop a “dashboard” for tropical Latin American countries that takes in weather data and produces predictive maps of the risk of dengue, Zika, chikungunya and other diseases and how those will change in the coming months due to weather patterns.
“That helps the government allocate scarce resources,” said McCord. “The dashboard will highlight the parts of the country where things are about to get worse, and quantifies ahead of time the requirements for extra staff, extra bed nets, extra medication so that the system can get ready for a surge of cases. That’s the kind of thing we’re creating right now.”
As director of the SDG Policy Initiative at UC San Diego, which uses the U.N. Sustainable Development Goals (SDGs) as a framework for bringing science to government, McCord is working alongside his colleagues in the School of Global Policy & Strategy on a number of fronts, including human health and wellbeing. They’ve partnered with the government of Paraguay on a two-year project to help the South American country close gaps to meeting SDG targets by 2030, particularly in health-related areas of adolescent fertility and obesity.
Understanding informal strategies for care
Recognizing that millions of low-income African Americans in the U.S. live without access to healthcare, Danielle Raudenbush, an associate professor of sociology in the School of Social Sciences at UC San Diego, spent more than three years conducting fieldwork in a public housing development working to understand the “informal strategies” members of this demographic turn to in order to access essentials like pharmaceutical drugs and medical equipment when standard healthcare is not available to them.
Her findings, which frame healthcare in the U.S. as a formal-informal hybrid system, offer key insights into the sources of disparities in health outcomes and became the basis for her book, “Health Care Off the Books: Poverty, Illness and Strategies for Survival in Urban America,” published by University of California Press in 2020.
“From population-level research, we know that on one level people belonging to that group face greater obstacles to accessing healthcare. We also know that they also have much higher rates of lots of different health problems. But we have this unanswered question, which is if they’re sick and they’re not able to access care, then what are they doing?” said Raudenbush. “So, the underlying question is, in the face of these challenges, how is the healthcare system functioning for this population?”

Now, she’s applying that same question to research right here in San Diego, investigating the effect that life in the border region has on the healthcare experiences of Mexican immigrants. So far, she’s found that those who are lawfully present and can cross back and forth across the border are strategically combining healthcare services in the U.S. and Mexico. In many cases, they choose to cross the border because of a dissatisfying experience in the U.S., and because care in Mexico is cheaper and more patient oriented. She sees this alternative option as a source of empowerment.
“There’s this kind of subgroup of people who are integrated in the U.S. healthcare system; they have insurance, they have what we call a usual source of care, so they have a clinic they go to or they have a primary care doctor, and yet they still at times go to Mexico for health services,” said Raudenbush.
Raudenbush, who comes from a mixed-race background, says that her exposure to both a primarily white upper-middle-class world and a primarily Black working-class world from a young age drove her to understand why disparities exist among certain populations. Health, she says, is fundamental to every aspect of people’s lives.
“That is why I’m driven to do this,” said Raudenbush. “I think until we really understand the roots of health inequality, until we really understand how people are getting care, or are not getting care, or the informal strategies they’re using, we won’t be able to effectively address these problems.”
Mailing at-home tests to increase cancer screening
For the past three years, at-home tests that screen for colorectal cancer have been arriving by mail to members of low-income and medically underserved communities in San Diego. That’s thanks to a National Cancer Institute-funded project co-led by María Elena Martínez, the Sam M. Walton Endowed Chair for Cancer Research at UC San Diego, and a team of researchers. Accelerating Colorectal Cancer Screening and Follow-up Through Implementation Science (ACCSIS) aims to close a startling disparity: that individuals from certain racial and ethnic groups, recent immigrants, the uninsured and those from low socioeconomic status groups are more heavily impacted by cancer, in part due to low screening rates.
A champion in the field of cancer disparities, Martínez, who also is a professor at the Herbert Wertheim School of Public Health and Human Longevity Science at UC San Diego and associate director, population science, disparities and community engagement for Moores Cancer Center at UC San Diego Health, has served on a number of national committees aimed at reducing inequities in cancer prevention and treatment for underserved populations.
In 2016, Martínez was named to then-Vice President Joe Biden’s Blue Ribbon Panel for the Cancer Moonshot Initiative to accelerate cancer research. In this role, Martínez led the charge on the panel’s recommendation that the initiative address low rates of colorectal cancer screening among historically marginalized groups.

“We made it a point to say you can continue doing what most research does, but if you don’t address the needs of lower-income and underserved communities, you will not change the existing inequities,” said Martínez.
With more than a year remaining in the study, Martínez and her team continue to implement the screening trial with the knowledge that the results of this study could be more broadly applied to other types of screenings such as cervical cancer. The ACCSIS team is working with Federally Qualified Health Centers, the primary care providers of uninsured and underinsured individuals, with the hope that their findings can be used as a blueprint for increasing cancer screening rates in the future.
She believes that the collaborative culture among researchers at UC San Diego is unparalleled, and is vital to addressing complex challenges like health inequities.
“It isn’t just a saying—it really is a collaborative culture. The common theme for us has been equity, inclusion, addressing disparities. It’s an easy area to get collaboration around because it’s something that we all buy into. It’s not just about collaborating around a hypothesis or theory—it’s about a bigger piece of the picture. It’s incredible,” Martínez said.
"It’s not just about collaborating around a hypothesis or theory—it’s about a bigger piece of the picture. It’s incredible."
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.