Bipolar Patients’ Brain Cells Predict Response to Lithium
Study among first to show how manic-depressive disorder affects neurons
Published Date
By:
- Scott LaFee
Share This:
Article Content
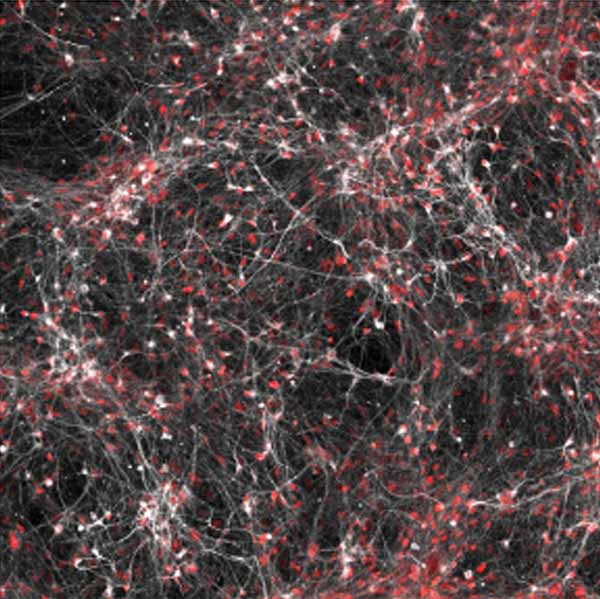
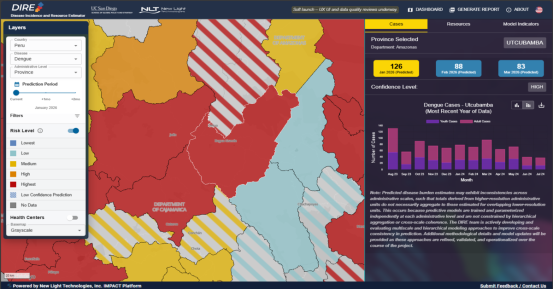
Neurons (white/red) from a subset of bipolar patients show changes in their electrical activity in response to lithium. Photo by Salk Institute
The brain cells of patients with bipolar disorder, a manic-depressive illness characterized by severe swings in mood, energy and ability to carry out daily tasks, are more sensitive to stimuli than other people’s brain cells, reports an international team of scientists headed by researchers at Salk Institute for Biological Studies and University of California, San Diego School of Medicine.
The finding, published in the October 28 online issue of Nature, is among the first to show at a cellular level how the bipolar disorder affects the brain, including why some patients respond to treatment with lithium while others don’t.
“Researchers hadn’t all agreed that there was a cellular cause to bipolar disorder so our study is important validation that the cells of these patients really are different,” said Rusty Gage, PhD, a professor in Salk’s Laboratory of Genetics and senior author of the study,
Bipolar disorder affects more than 5 million Americans. It cannot be cured, and is often difficult to treat. If patients’ severe mood swings aren’t improved with lithium, a long-standing drug widely used to treat bipolar disorder and other mental illnesses, doctors may resort to piecing together treatment plans using antipsychotic drugs, antidepressants and mood stabilizers. These remedies can ease depressive or manic swings, but not both.
To study the underlying cause of bipolar disorder, the scientists collected skin cells from six bipolar patients, reprogrammed the cells to become stem cells and then coaxed the stem cells to develop into neurons. They then compared these derived neurons to neurons from healthy controls.
“Neurons are normally activated by a stimuli and respond,” said Jerome Mertens, PhD, a postdoctoral research fellow at Salk and first author. “The cells we have from all six bipolar patients are much more sensitive in that you don’t need to activate them very strongly to see a response.” In addition, the mitochondria – the energy-generating powerhouses inside the cells – were also more active.
Of the six patients in the study, three had responded to previous lithium treatment and three had not. The researchers investigated to see how their cells reacted to lithium, allowing some of the stem cell-derived neurons to grow in liquid containing lithium and then re-measuring how sensitive the cells were.
Although neurons from the two patient groups appeared identical and equally sensitive in initial testing, they behaved differently when exposed to the lithium. Cells from lithium-responder patients showed weakened excitability after growing in the lithium, but cells from patients who hadn’t been helped by the drug remained “hyperexcitable.”
“The stem cell-derived neurons were three to four times more electrically active than control cells and tended to burn themselves out,” said John Kelsoe, Jr., MD, professor of psychiatry at UC San Diego School of Medicine and a co-author of the study. “This was reversed by treatment with lithium, but only in cells that came from patients who had responded to lithium.”
The findings don’t explain why lithium works for some patients and not others, but offer a starting point for investigating additional differences between cells. The stem cell-derived bipolar neurons also provide a new platform to ask other questions about the disorder.
“Now that we have neurons that show differences in excitability, we can use these to screen for better drugs,” said Mertens. If a new drug, for instance, reverses the hyperexcitability at the cellular level, it would likely treat bipolar disorder in patients.
Researchers plan to next monitor affected cells for longer periods of time to see whether their hyperexcitability state is only an initial manic stage or long-lasting. “After a few months, it’s possible that this hyperexcitability becomes too much for the cell to handle and it crashes into a less excitable state,” said Gage. “That could signal the shift between the depression and mania that patients experience.”
Co-authors include Qiu-Wen Wang, Bo Yang and Yi Zheng, Jun Yao, Tsinghua University, China; Yongsung Kim, Diana X. Yu, Son Pham, Sheila Soltani, T.J. Eames, Simon T. Schafer, Leah Boyer, Maria C. Marchetto, Kenneth E. Diffenderfer, Salk Institute; Jian Zhang and Shuangli Mi, Chinese Academy of Sciences, China; John I. Nurnberger, Indiana University; Joseph R. Calabrese, Case Western Reserve University; Ketil J. Ødegaard, University of Bergen, Norway; Michael J. McCarthy, VA San Diego Healthcare System; Peter P Zandi, Johns Hopkins University; The Pharmacogenomics of Bipolar Disorder Study, Kristen J. Brennand, Mount Sinai School of Medicine and Caroline M. Nievergelt, UC San Diego.
Funding for this research came, in part, from the National Natural Science Foundation of China, the National Basic Research Program of China, the Engmann Family Foundation, the JPB Foundation, the Leona M. and Harry B. Helmsley Charitable Trust, the G. Harold and Leila Y. Mathers Charitable Foundation, the Glenn Foundation for Medical Research, the National Institute of Mental Health (grant U01 MH92758) and the Department of Veterans Affairs.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.