By:
- Deborah Bright
- Heather Buschman, Ph.D.
Published Date
By:
- Deborah Bright
- Heather Buschman, Ph.D.
Share This:
What’s in Your Gut?
Big data dump from the world’s largest citizen science microbiome project reveals how factors such as diet, antibiotics and mental health status can influence the microbial and molecular makeup of your gut
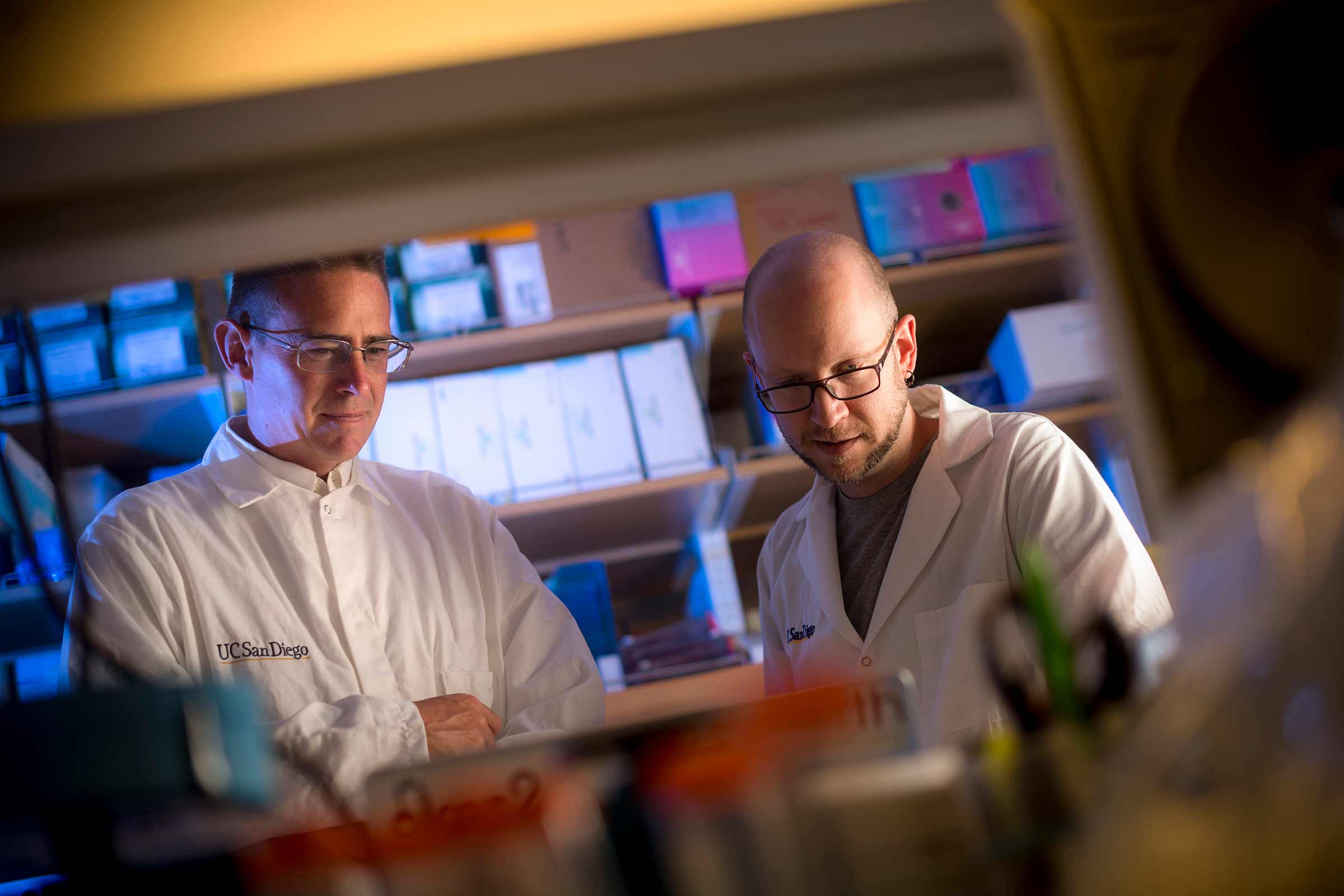
Rob Knight, UC San Diego professor of pediatrics and computer science and engineering, and postdoctoral researcher Daniel McDonald discuss data from The American Gut Project, which was published in an open-access journal earlier this week. Photos by Erik Jepsen/UC San Diego Publications
American journalist Michael Pollan meticulously rolled a cotton-tipped swab across a piece of used toilet paper. His sample was about to become the first of 15,096 that would be included in the first major publication of the American Gut Project—an ongoing citizen science effort boasting more than 10,000 participants from all over the world. The publication appeared in the open access journal mSystems earlier this week.
“It’s really amazing that over 10,000 people—members of the public who want to get involved in science whether or not they work in a lab or have a Ph.D.—have mailed their poop to our lab so that we can find out what makes a difference in somebody’s microbiome,” said Rob Knight, UC San Diego professor of pediatrics and computer science and engineering whose lab leads the project out of the UC San Diego Center for Microbiome Innovation.
UC San Diego professor of pediatrics and computer science and engineering Rob Knight, whose lab leads the project at the UC San Diego Center for Microbiome Innovation
For $99, budding citizen-scientists receive a kit containing swabs, which they are instructed to dab on a used piece of toilet paper and mail to the Knight lab at UC San Diego if they are located in the United States, the Department of Twins Research at King’s College if they are located in the United Kingdom, or the Australian Centre for Ecogenomics at the University of Queensland in Australia.
Along with the sample, each participant also answers a voluntary survey related to general health status, disease history and lifestyle, including diet. They can also choose to participate in an online forum called Gut Instinct, which enables participants to share their lifestyle-based insights with one another. Once their sample is processed, the participant receives a standard report informing them of “what’s in their gut.”
“Here were the names of the hundreds of bacterial species that call me home,” said Pollan of his printout, in a piece he wrote for The New York Times. “In sheer numbers, these microbes and their genes dwarf us. It turns out that we are only 10 percent human: for every human cell that is intrinsic to our body, there are about 10 resident microbes— including commensals (generally harmless freeloaders) and mutualists (favor traders) and, in only a tiny number of cases, pathogens. To the extent that we are bearers of genetic information, more than 99 percent of it is microbial. And it appears increasingly likely that this ‘second genome,’ as it is sometimes called, exerts an influence on our health as great and possibly even greater than the genes we inherit from our parents. But while your inherited genes are more or less fixed, it may be possible to reshape, even cultivate, your second genome.”
The American Gut Project is the largest microbiome study ever to be published and it validates citizen science as a feasible model for engaging the public on scientific topics. Among the observations made by the team of scientists at the UC San Diego Center for Microbiome Innovation is that the number of plants in a person’s diet is a factor in the diversity of their gut microbiome.

The American Gut Project Mini-Symposium was held May 15 in celebration of the publication.
The project was launched in November of 2012 as a subset of the Earth Microbiome Project to discover the kinds of microbes and microbiomes “in the wild.” As of the middle of last year, the project included microbial sequence data from 15,096 samples from 11,336 human participants representing primarily the United States, United Kingdom and Australia, along with 42 other countries or territories, making the dataset the largest public reference database of the human gut microbiome.
“We observed a much greater microbial diversity than previous smaller studies found, and that suggests that if we look at more populations, we’ll see more diversity, which is important for defining boundaries of the human microbiome,” said Daniel McDonald, Ph.D., scientific director of the American Gut Project and postdoc at the UC San Diego School of Medicine.
To tease out the identities of the bacteria living in a participant’s mixed sample, the American Gut Project team sequences a genetic marker unique to bacteria and archaea. Called 16S rRNA, this molecule acts as a sort of barcode for these microbes. For thousands of the samples, they also used metabolomics methods to identify the non-living molecules and chemicals present, and shotgun metagenomics to read out all of the genes.
Emerging trends
All of the data collected by the American Gut Project are publicly available, without participants’ identifying information. This open access approach allows researchers around the world to mine the data for meaningful associations between factors such as diet, exercise, lifestyle, microbial makeup and health. Here are a few observations that have emerged so far:
Diet. The number of plant types in a person’s diet plays a role in the diversity of his or her gut microbiome—the number of different types of bacteria living there. No matter the diet they prescribed to (vegetarian, vegan, etc.), participants who ate more than 30 different plant types per week (41 people) had gut microbiomes that were more diverse than those who ate 10 or fewer types of plants per week (44 people). The gut samples of these two groups also differed in the types of molecules present.

The May 15 Mini-Symposium featured talks by some of the main authors on aspects of the project they found most interesting.
Antibiotics. The gut microbiomes of American Gut Project participants who reported that they took antibiotics in the past month (139 people) were, as predicted, less diverse than people who reported that they had not taken antibiotics in the last year (117 people). But, paradoxically, people who had taken antibiotics recently had significantly greater diversity in the types of chemicals in their gut samples than those who had not taken antibiotics in the past year.
The participants who ate more than 30 plants per week also had fewer antibiotic resistance genes in their gut microbiomes than people who ate 10 or fewer plants. In other words, the bacteria living in the guts of the plant-lovers had fewer genes that encode the molecular pumps that help the bacteria avoid antibiotics. This study didn’t address why this might be the case, but the researchers think it could be because people who eat fewer plants may instead be eating more meat from antibiotic-treated animals or processed foods with antibiotics added as a preservative, which may favor the survival of antibiotic-resistant bacteria.
Mental health. The American Gut Project researchers also examined the gut microbiomes of 125 people who reported having a mental health disorder, such as depression, schizophrenia, post-traumatic stress disorder (PTSD) or bipolar disorder. They matched each of these participants to individuals who did not have a mental health disorder, but did have other major factors in common, such as country, age, sex and body mass index. The team found that people with a mental disorder had more in common with other people with mental disorders, in terms of the bacteria makeup of their gut microbiomes, than they did with their mentally healthy pairs. The observation held true in both U.S. and UK populations, in males and females, and across age groups. In addition, the research team found some indications that specific bacteria types may be more common in people with depression than people who do not have the condition.
“The Man Who Saw Inside Himself”
One American Gut Project participant sampled himself at multiple time points before and after colorectal surgery—Larry Smarr, Ph.D., founding director of the California Institute for Telecommunications and Information Technology (CalIT2) and Harry E. Gruber Professor of Computer Science and Engineering at UC San Diego.

Smarr speaks about his data at the American Gut Project Mini-Symposium on May 15.
“We were blown away by the changes we observed in his pre- and post-microbial configuration,” McDonald said. “They exceeded the span of microbial diversity associated with the American Gut Project population. After surgery, Smarr’s samples most closely resembled those of patients in the intensive care unit. In fact, when his samples were placed on a map, the distance between the samples immediately prior to and following the surgery was almost identical to the distance between a marine sediment sample, and one from the soil under a land plant.”
Dramatic state changes like this aren’t even observed in cases of extreme diets, McDonald said. “We don’t know how to modulate the microbiome. People generally assume you can over short timescales by eating differently, but those effects tend to be small, not massive.”
Looking ahead
“The AGP is dynamic, with samples arriving from around the world daily,” said Knight. “The analysis presented here represents a single snapshot, but we’re going to beyond making maps of the microbiome to making a microbiome GPS that tells you not just where you are on that map, but where you want to go and what to do in order to get there in terms of diet, lifestyle or medications.”
At a celebration of the milestone publication on May 15, the team announced an expansion of the project called “The Microsetta Initiative,” which will serve as an umbrella for sites that can receive samples in countries around the world.

At the May 15 event, Chancellor Khosla welcomed the audience and talked about the importance of this project in discovering and better understanding our microbes and microbiomes.
According to McDonald, living datasets like this will allow researchers to document the slow but steady global homogenization driven by increased travel, lifespans, and access to similar diets and therapies, including antibiotics.
Future example applications of the AGP living dataset include comparing the AGP population to samples collected from a fecal transplant study and an infant microbiome time series.
How to participate
To learn more or to participate in the American Gut Project, visit AmericanGut.org.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



