Transforming Medical Education to Save Lives
Award-Winning Paper Impacts How Physicians Learn
Published Date
Story by:
Media contact:
Share This:
Article Content
Resident physicians are learning to make their mark with the help of innovative technology that transforms traditional training into a more user-friendly experience, and a recent study is paving the way for this new approach to education in the field of cancer treatment. The research was recognized at both CHI 2024 and ACM DIS 2024, with one paper receiving an honorable mention award—an achievement reserved for the top 5% of submissions. The study was led by Ph.D. student Matin Yarmand and Professor Nadir Weibel from UC San Diego’s Design Lab and Department of Computer Science in the Jacobs School of Engineering, in collaboration with UC San Diego School of Medicine. The study brings together physicians, radiation oncology residents, and designers to prioritize human-centered design in healthcare innovation.
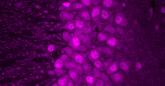
At the center of this innovation is the process of “contouring,” in which doctors outline treatment areas, like tumors, on medical images to guide radiation therapy.
Traditionally, contouring training has involved faculty using stationary desktop computers to guide residents through the process of outlining treatment zones on medical images. Instructors typically do this by using a mouse to click and outline areas on the body, while having the resident watch their workflow and later mimic the process. This method can be difficult and time consuming, as it is hard to draw accurately with a mouse. Additionally, simply watching an instructor contouring does not give medical students enough opportunity to practice and build skills.
In examining the issues with traditional training, the team began to imagine what it might look like to learn to contour using a mobile device with flexible and independent training. Touch-based tablets and phones could open up new possibilities, allowing users to draw with a finger or stylus, while also making the learning process faster, more natural, and portable. These devices also offer the ability to provide fast feedback on residents’ contouring sessions.

Yarmand and Weibel’s research shows that radiation oncology is complicated and prone to errors. These mistakes impact patient survival and also waste time and resources, showing the need for better systems in healthcare. “In healthcare settings, when you work with real patients in high-stake settings, errors can lead to a decrease in patient safety,” says Yarmand. “And in drastic cases with radiation oncology, patient survival.”
The team recognized from the outset that collaboration was essential to creating a meaningful solution. They recognized that engaging physicians throughout the entire process was essential for the technology to effectively address their needs and create meaningful impact. They focused on designing a system that fits seamlessly into the workflows of physicians and residents—an embodiment of human-centered design in action. The team conducted interviews and workshops from the beginning, incorporating feedback at every stage.
The team aimed to improve not only the quality of training but also its accessibility. Training quality often depends on patient case numbers, creating gaps between rural and urban facilities. By mobilizing training, the system helps bridge these gaps and gives all residents more equal opportunities.
“Hopefully, we can close this quality gap a little bit more,” says Yarmand. “We can try to achieve this future where there is equally ideal treatment for patients with cancer.”
The system has been fully developed and is currently being used in a nationwide study, which has been underway for three months. The study includes around 30 residents from across the country who are enrolled in the system and periodically provide feedback on their progress in radiation oncology training. With this major part of the system already being studied, additional capabilities are nearing completion, with plans for further testing soon.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.