By:
- Cynthia Dillon
Published Date
By:
- Cynthia Dillon
Share This:

Photo by Erik Jepsen/UC San Diego Publications
To Wear a Mask or Not, Is Not the Question; Research Indicates It’s the Answer
A team of scientists from the University of California San Diego, Caltech and Texas A&M remotely put their heads together to analyze the transmission pathways of COVID-19. Their study confirms that face coverings determine the pandemic’s trends and significantly reduce the number of infections.
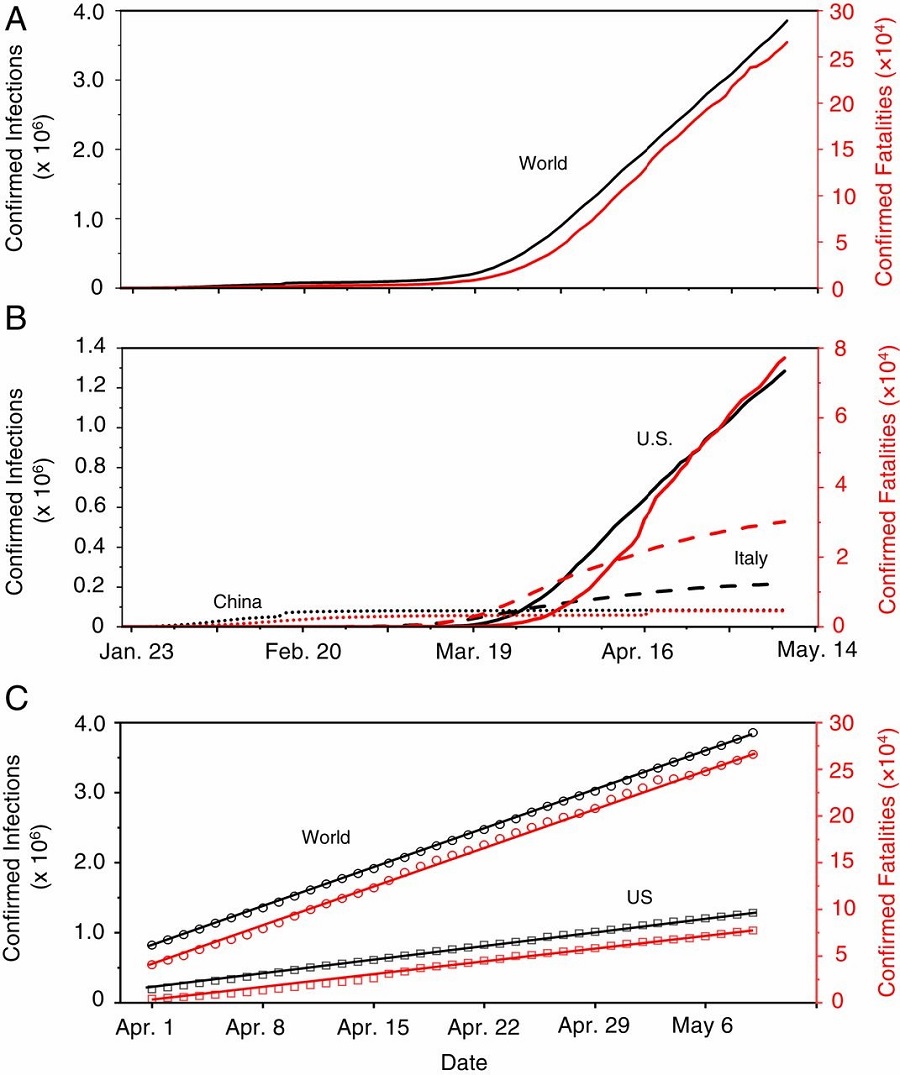
Figure 1. Distinct global trends of the COVID-19 pandemic. Figure courtesy of the research team.
Examining trends and mitigation measures in three epicenters—Wuhan, China; Italy and New York City—the scientists’ study, published recently in PNAS, shows that airborne transmission is the highly virulent and dominant route for spreading COVID-19. At the same time, the study shows that other mitigation measures, such as social-distancing and shelter-in-place, insufficiently protect the public.
“Our work also highlights the necessity that sound science is essential in decision-making for the current and future public health pandemics,” said UC San Diego’s Nobel Laureate in chemistry and Distinguished Professor Mario Molina.
The study shows that, between April 6 and May 9 in Italy and New York City mandated face coverings significantly reduced the number of infections by more than 140,000 between the two epicenters.
The scientists quantified the effects of face-covering by projecting the number of infections based on the data before Italy and New York City implemented the use of face masks on April 6 and April 17, respectively (see Figure 2A). The inability of social distancing, quarantine and isolation alone to curb the spread of COVID-19 is also evident from the linearity of the infection curve prior to the onset of the face-covering rule in Italy and in New York City on those dates (see Figure 2 B and C).
The scientists also compared the numbers of daily new cases between New York City and the U.S. from March 1 to May 9 (Figure 3). The daily numbers of newly confirmed infections show a sharp increase in late March and early April. After April 3, the only difference in the regulatory measures between New York City and the U.S. lies in the city’s April 17 face-covering rule.
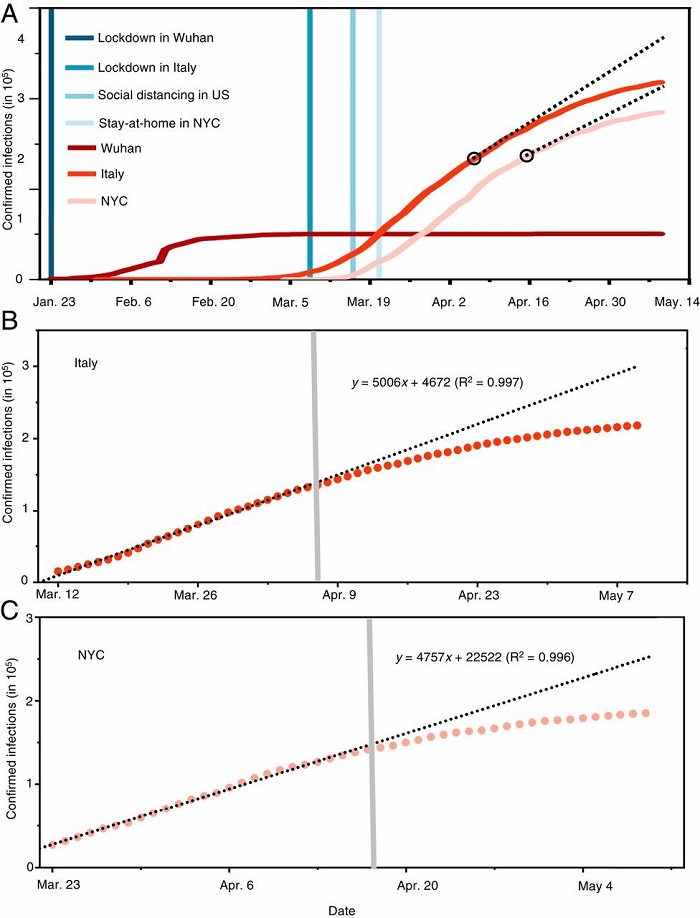
Figure 2. The evolving epicenter from Wuhan, to Italy, to NYC. (A) Comparison of the trends and mitigation measures between Wuhan, Italy, and NYC in 2020. The vertical lines mark the date for implementing mitigation measures. The two black circles label the dates when face-covering was implemented. The black dashed lines represent the projection without face-covering based on linear regression of data prior to implementing this measure. (B) Linear regression of the number of confirmed infections for data prior to implementing face-covering in Italy. The shaded vertical line denotes the date when face-covering was implemented in northern Italy. (C) Linear regression of the number of confirmed infections for data prior to implementing face-covering in NYC. The shaded vertical line denotes the date when face-covering was implemented in NYC. In B and C, the circles are reported values, and the dotted line represents fitting and projection of the confirmed infections before and after face-covering, respectively. Figure courtesy of the research team.
According to the researchers, the decreasing rate in the daily new infections in New York City with mandated face-covering sharply contrasts with the United States’ mask-free measures of social-distancing and shelter-in-place, further confirming the importance of face-covering in intervening the virus transmission.
“We conclude that the wearing of face masks in public corresponds to the most effective means to prevent inter-human transmission, and this inexpensive practice, in conjunction with simultaneous social distancing, quarantine and contact tracing, represents the most likely fighting opportunity to stop the COVID-19 pandemic,” said Renyi Zhang, distinguished professor of atmosphere science at Texas A&M.
Molina agreed. “The unique function of face-covering to block atomization and inhalation of virus-bearing aerosols accounts for the significantly reduced infections in China, Italy and New York City (Figs. 1–3), indicating that airborne transmission of COVID-19 represents the dominant route for infection,” stated Molina.
There are several ways for viruses to be transmitted from person to person. Infected individuals produce microscopic, virus-bearing particles that spread when they cough, sneeze, breathe and talk. This viral shedding produces large droplets and small aerosols—suspensions of particles in the atmosphere—which disperse and stay in the air at differing rates and for various times. They also have characteristic deposition patterns along the human respiratory tract.
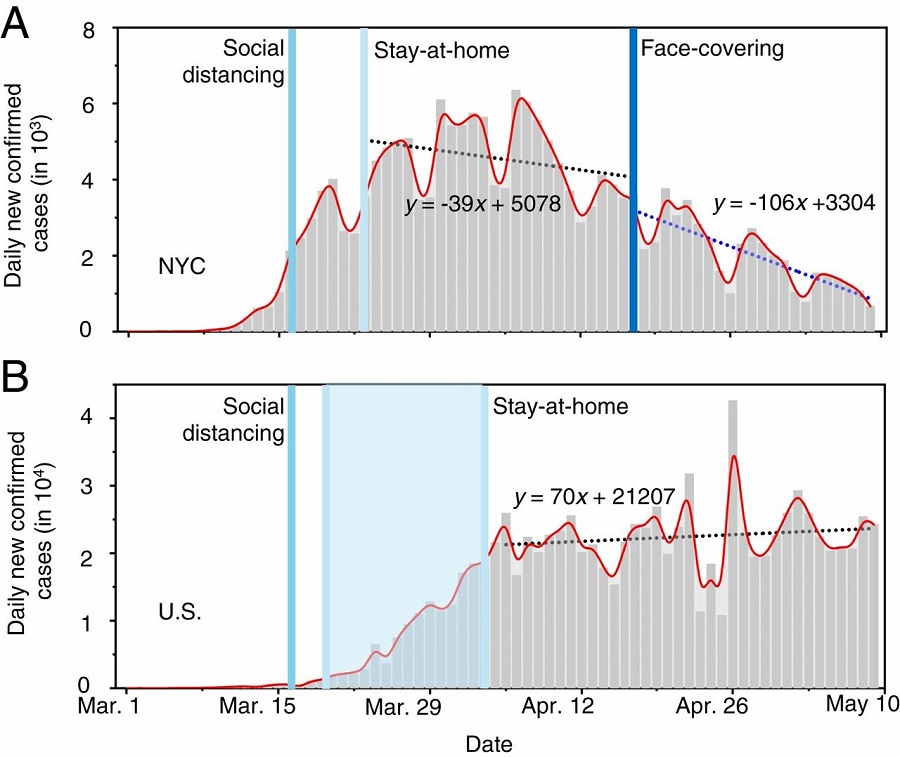
Figure 3. Contrasting the trends of new infections between NYC and the U.S. Daily new confirmed infections in (A) NYC and (B) the U.S. The dotted lines represent linear fitting to the data between April 17 and May 9 in NYC and between April 4 and May 9 in the U.S. In B, the number in NYC was subtracted from that in the U.S. The vertical lines label the dates for social distancing, stay-at-home orders and mandated face-covering. Figure courtesy of the research team.
“With typical nasal breathing, inhalation of airborne viruses leads to direct and continuous deposition into the human respiratory tract. In particular, fine aerosols penetrate deeply into the respiratory tract and even reach other vital organs,” explained Molina, adding that viral shedding is dependent on the stages of infection and varies between symptomatic and asymptomatic carriers.
Previous experimental and observational studies on inter-human transmission have shown that aerosols play a significant role in transmitting many respiratory viruses, including influenza virus, SARS-CoV-1 and Middle East Respiratory Syndrome coronavirus (MERS-CoV). For example, airborne coronavirus MERS-CoV exhibited a strong capability of surviving, but it decayed quickly. Recent experimental studies on the stability of SARS-CoV-2 show that it remains infectious for hours in aerosols and up to a few days on surfaces.
Molina, Zhang and their colleagues demonstrated the contribution of airborne transmission to the COVID-19 outbreak by comparing the pandemic’s trends and mitigation measures worldwide, and by considering the virus’ transmission routes (see Figure 4).
The COVID-19 outbreak is significantly more pronounced than that of the 2002–2003 SARS epidemic, and the disease continues to spread at an alarming rate worldwide, despite extreme measures taken by many countries to constrain it. The enormous scope and magnitude of the COVID-19 outbreak reflect not only a highly contagious nature but also exceedingly efficient virus transmission. While the mechanisms to spread the virus remain uncertain, current epidemiological and experimental evidence implicates airborne transmission via aerosols as a potential route for spreading the disease.
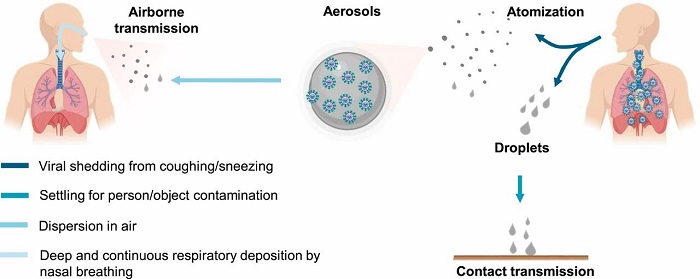
Figure 4. Transmission of COVID-19. Figure courtesy of the research team.
The scientists explain that several parameters likely influence the microorganism’s survival and delivery in air, including temperature, humidity, microbial resistance to external physical and biological stresses, and solar ultraviolet radiation. Transmission and infectivity of airborne viruses are also dependent on the size and number concentration of inhaled aerosols, which regulate the amount or dose and pattern for respiratory deposition.
The novel coronavirus outbreak, which was declared a pandemic by the World Health Organization (WHO) on March 11, 2020, has infected more than eight million people and caused more than 400,000 fatalities to date. Intensive efforts are taking place globally to establish effective treatments and develop a vaccine for the disease, including efforts by several UC San Diego researchers.
This work was supported by the Robert A. Welch Foundation with a grant (no. A-1417) and a fellowship.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



