Survival Is a Mixed Matter for Deadliest of Pancreatic Cancers
UC San Diego scientists find that quality and mix of collagen in pancreatic ductal adenocarcinoma tumors determines whether prognosis is poor or very poor
Story by:
Published Date
Article Content
Pancreatic ductal adenocarcinoma (PDAC) is the most common and most lethal form of pancreatic cancer. The overall 5-year survival for patients with PDAC is just 7.1 percent.
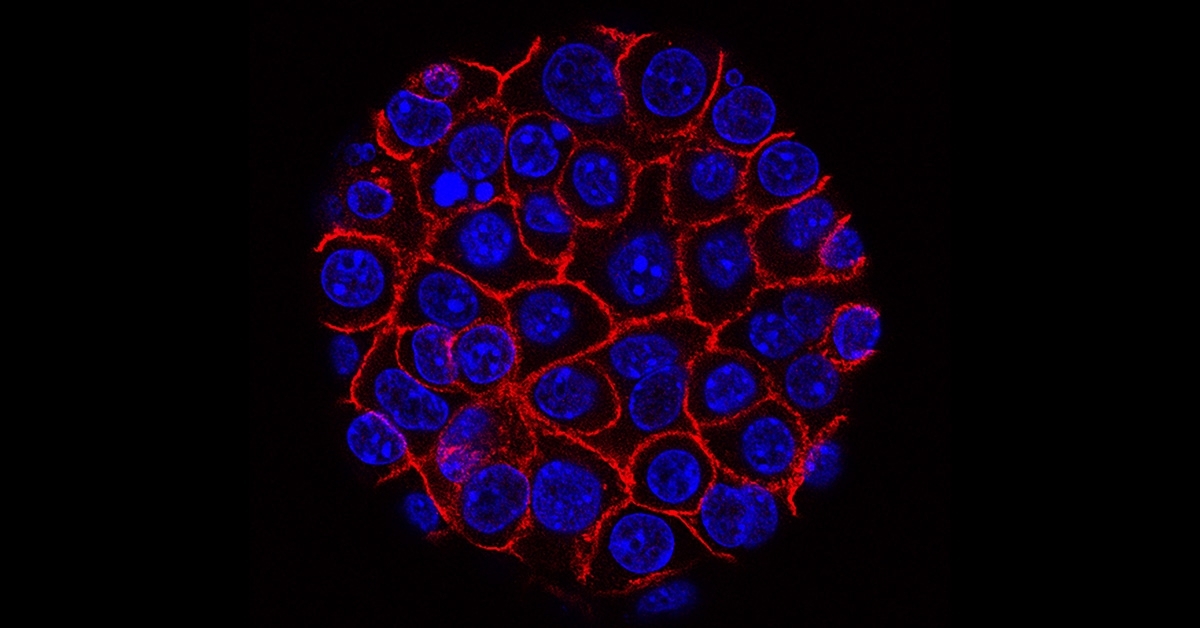
All cancers are different. A unique feature of PDAC is extensive tumor desmoplasia or fibrous connective tissue within the tumor, which is caused by infiltration of the tumor mass by fibroblasts and the extracellular matrix they secrete. The main component of the matrix is type I collagen or Col 1, a protein broadly used in the body to form the basic structure of bone, skin, blood vessels and connective tissues.
The effect of Col 1 on PDAC development and its response to therapy has been a matter of intense debate among researchers, with some arguing that Col 1 promotes tumor growth and spread and others contending that it restricts tumor growth and protects the cancer cells from immune attack.
In a new study, published October 5, 2022, in Nature, co-first authors Hua Su, PhD, a postdoctoral fellow in the lab of senior author Michael Karin, PhD, Distinguished Professor of Pharmacology and Pathology at University of California San Diego School of Medicine, and Fei Yang, PhD, a scientist working with Beicheng Sun, MD, PhD, at Nanjing University School of Medicine, settle the debate by showing that it is not the amount of Col 1 present in the tumor that matters, but its quality and nature.
Specifically, they report that Col 1 that has been cleaved by matrix metalloproteases (enzymes that break down matrix proteins, such as collagen) stimulates tumor growth while intact and non-cleaved Col 1 inhibits tumor growth.
“Moreover,” said Su, “cleaved Col 1 activates a signaling pathway that stimulates energy production in pancreatic cancer cells by binding to a receptor protein called DDR1. Non-cleaved Col 1 inhibits this pathway by inducing the degradation of DDR1.”
The research was conducted using mice models and a novel culture system in which PDAC cells were plated on extracellular matrix that contained either cleaved or non-cleaved Col 1.
The authors said the findings have important clinical implications.
The relative amounts of cleaved versus non-cleaved Col 1 in the human PDAC stroma or connective tissue strongly affect patient survival after surgical resection. Patients whose tumors were enriched in cleaved Col 1 and whose cancerous cells expressed high levels of DDR1 fared poorly, with most succumbing to their disease within two years of surgery.
This patient group represented 75 percent of the 106 patients analyzed as part of the study, using cancer specimens provided by Beicheng Sun, MD, PhD, and colleagues at the Affiliated Drum Tower Hospital of Nanjing University Medical School in China.
In contrast, the 25 percent of patients whose tumors mainly contained non-cleaved Col 1 with low levels of DDR1 expression experienced much better survival prospects.
“This work is important because it provides a simple way for patient stratification and suggests that patients with high levels of cleaved Col 1 and DDR1 expression need more aggressive post-surgery treatments,” said Karin.
“It also provides evidence that the most effective therapy for this group of patients should include inhibitors of DDR1 or key components of its signaling pathway whose activation results in increased number of mitochondria, the cellular power plants, in PDAC cells.”
In addition to DDR1 inhibitors not yet in clinical practice, the authors suggested another treatment option, shown to be effective in PDAC-bearing mice, is the U.S. Food and Drug Administration approved antibiotic tigecycline, which can inhibit mitochondrial protein synthesis and decrease the number of energy-producing PDAC mitochondria.
Co-authors include: Rao Fu, Nanjing University Medical School; Brittney Trinh, Nina Sun, Junlai Liu, Jacopo Baglieri, Nachanok Sinchai, Jeremy Siruno, Stephen Dozier, Ajay Nair, Aveline Filliol, Sara Brin Rosenthal, Jennifer Santini, Anthony Molina, Robert F. Schwabe, Andrew M. Lowy and David Brenner, all at UC San Diego; and Avi Kumar and Christian M. Metallo, Salk Institute.
Funding for this research came, in part, from the National Institutes of Health (grants R01CA211794, R37AI043477, P01DK098108, U01AA027681, U01CA274295), the Padres Pedal the Cause/C3, the Cancer Center Support Grant and UC San Diego School of Medicine Microscopy Core.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.