Researchers Boost Body’s Inflammation-Reduction Mechanism to Combat Obesity-Fueled Disease
Published Date
By:
- Bonnie Ward
Share This:
Article Content
Researchers at University of California, San Diego School of Medicine and University College Dublin (UCD) have found that augmenting a naturally occurring molecule in the body can help protect against obesity-related diseases by reducing inflammation in the fat tissues. The study, published June 4 in the journal Cell Metabolism, focused on liver and kidney diseases, but the researchers believe it could lead to a new therapeutic approach for a variety of obesity-fueled conditions.
“This is a new way of reducing inflammation and protecting organs, using a compound that’s already produced by the body,” said co-senior author Kumar Sharma, MD, a professor of medicine and director of the Center for Renal Translational Medicine at UC San Diego School of Medicine. “Essentially, we’re boosting the body’s natural response for reducing inflammation and showing the benefit in obesity-driven diseases.”
Catherine Godson, PhD, co-senior author and director of the UCD Diabetes Complications Research Centre in UCD School of Medicine and UCD Conway Institute, said the study’s findings demonstrate the value and potential impact of fundamental research. “Drawing on collaborative expertise in synthetic chemistry, molecular biology and translational medicine, the team has produced findings with significant potential to reduce inflammation, a critical driver of the devastating consequences of obesity-related diseases,” she said.
In the body, inflammation is normally a natural healing response to infection or injury. “You get a recruitment of white blood cells that fight off the infection or work to heal the injury,” explained first author Emma Borgeson, PhD, a postdoctoral fellow at UC San Diego and UCD. “It is a good thing. It’s only when the inflammation becomes chronic that it can cause disease to occur.”
Borgeson said that a family of lipids, known as specialized pro-resolving mediators (SPMs), are the body’s natural shut-off mechanism for inflammation. “The process of telling the white blood cells to ‘calm down, you don’t have to be inflamed anymore’ is called inflammatory resolution and that’s what the SPMs induce.”
In the study, the research team focused on an SPM called lipoxin A4, which has previously been found to reduce inflammation in kidney disease caused by ureteral obstruction. Working with an obese mouse model, the researchers gave the mice a synthetic version of lipoxin A4 to boost the amount of the natural substance already in their systems. The results showed significant disease improvement, primarily by affecting fat tissue.
“The mice had been on a high-fat diet for three months and were already showing evidence of organ dysfunction, particularly in the liver and kidneys,” said Sharma. “The lipoxin A4 compound was given in an interventional manner for the last two months of the diet regime. We found that it significantly reduced inflammation in the fat tissues and improved kidney and liver disease. Overall, the lipoxin protected against obesity-induced organ damage, without noticeable side-effects.”
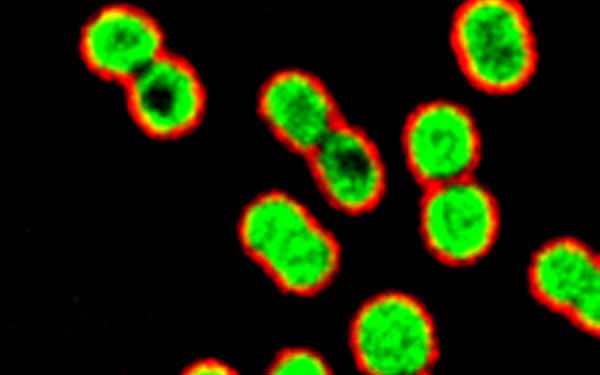
Borgeson said one of lipoxin A4’s key mechanisms of action is to switch the phenotype of the fat tissue macrophage cells from inflammatory to anti-inflammatory. This increases production of the protective protein Annexin-A1, reduces production of inflammatory cytokines and restores normal cell function. “This cascade of molecular actions reduces inflammation in the fat tissues and produces a systemic domino-effect with dramatic benefit in multiple organs.”
The next step will be to explore the effects of lipoxin A4 in samples of human fat tissue, said Borgeson, who has already started this work as a guest researcher at the Sahlgrenska Academy Hospital in Sweden. “The question is, ‘Can lipoxin modulate human cells in a similar fashion as it did in the mice?’” The research is at an early stage, but Borgeson said preliminary results are promising.
“Our ultimate hope would be to use these findings to create a lipoxin-based drug for obese people to help protect them against associated illnesses, such as kidney and liver disease,” she said. “It wouldn’t be a traditional ‘diet drug.’ It doesn’t reduce body weight. However, it may help obese patients avoid the dangers of obesity and inflammation-fueled disorders and remain relatively healthy.”
Co-authors include Andrew M.F. Johnson, Yun Sok Lee, and Gulam Hussain Syed, UC San Diego; Andreas Till, UC San Diego and University Clinic Bonn, Germany; Syed Tasadaque Ali-Shah, and Patrick J. Guiry, University College Dublin; Jesmond Dalli, Romain A. Colas, and Charles N. Serhan, Harvard Medical School.
Disclosure: Co-senior author Kumar Sharma, MD, a UC San Diego professor, is co-founder of ClinMet, Inc., in which he holds equity interest. Sharma is on the Board of Directors of the company and serves as a scientific advisor. There is technology licensed from UC San Diego to ClinMet which provides pharmaceutical companies with clinically relevant and practical insight into drug response and safety for renal and cardiovascular diseases, obesity and diabetes. In addition, Sharma's spouse is co-founder, president and chief operating officer of ClinMet, and holds equity interest.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



