Qualcomm Institute’s CARI Therapeutics Awarded NIH Grant for Opioid Sensor
Published Date
By:
- Tiffany Fox
Share This:
Article Content

CARI Therapeutics CEO and co-founder Patrik Schmidle, who is a co-principal investigator on the project.
Researchers at the University of California San Diego, in collaboration with CARI Therapeutics of the University's Qualcomm Institute Innovation Space, have begun development of a biosensor that will detect the presence of opioids in patients in recovery and might ultimately transform the way opioid use disorders are diagnosed, monitored, and treated.
According to a recent reportfrom The New York Times, more than 52,000 people in the U.S. died from a drug overdose in 2015, usually from opioids like heroin and Fentanyl. Estimates for 2016 top 60,000 drug overdose deaths, which exceeds the number of deaths from car crashes, HIV, and gunshot wounds.
“Clearly this crisis is claiming the lives of tens of thousands of people every year, and indications are it’s only going to get worse before it gets better,” says Patrik Schmidle, a co-principal investigator on the project and CEO/co-founder of CARI Therapeutics, which is based in the Qualcomm Institute Innovation Space. “There are more than 2.5 million people in the U.S. who suffer from an opioid use disorder, but what has really accelerated the crisis is the number of overdoses that occur every day, and in every year.”
The work is being funded, in part, by a $235,000 Phase I STTR (Small Technology Transfer Innovation Research) grant from the National Institute of Drug Abuse, a branch of the National Institutes of Health. Schmidle will lead the project in collaboration with Assistant Professor Drew Hall of the UC San Diego Department of Electrical and Computer Engineering (where he leads the Biosensors and BioElectronics Group), as well as Dr. Carla Marienfeld, an addiction psychiatrist with UC San Diego Health who specializes in treating patients with substance abuse disorders.
In Phase I of the project, the researchers aim to create a prototype of the injectable sensor, which will detect the presence of opioids (in this case, morphine) in interstitial fluid — the fluid that surrounds human cells and provides the cells with nutrients while also removing waste. Hall, who is also an affiliate of the Qualcomm Institute, describes the sensor as “about the size of a grain of rice and injected subcutaneously, where it has direct access to many physiologically relevant biomarkers.” Measurements are taken periodically throughout the day and the results are then communicated wirelessly to a worn device, such as a smartwatch or a smartphone.
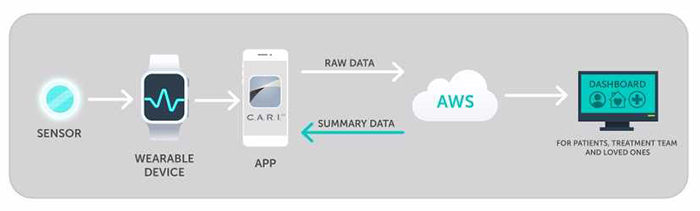
An illustration of the data flow for the proposed opioid sensor.
The project is related to a previous National Science Foundation-funded effort, also led by Schmidle, that created a technology platform for alcohol monitoring and similarly consists of a biosensor connected to a mobile app.
“Conceptually, you can think about this opioid sensor as similar to continuous glucose monitoring, which tracks glucose levels continuously throughout the day in as close to real-time as possible,” explains Schmidle. He says such a device would be superior to the current standard of care for substance use disorders: the urine test, or sometimes a blood test, which is administered to people enrolled in treatment programs.
“Certainly the people who want to circumvent the tests will try to find ways to do that, but the biggest challenge of the current method is it’s demeaning and very inconvenient for people,” especially if the tests must be supervised and/or random, Schmidle notes.
But more importantly, urine and blood tests involve a lag time — a lag time that can prove deadly if patients overdose and don’t receive treatment soon enough.
With the patient’s consent and with the help of the patient’s treatment team, “the hope is that we can speed up the process of identifying when people are relapsing and get them help before they overdose,” says Schmidle. “Our goal is that once we create a proof-of-concept for morphine, we can detect multiple substances with one sensor, including heroin and prescription pain medications.”
Adds Dr. Marienfeld: “Every day I see patients in my clinic struggling with the aftermath of their opioid use. They are getting mixed messages from their family, friends, and society about how to address their problem. To start, we know that behaviors do not change unless we pay attention to them. We see this with weight loss or smoking.
“Improved detection of opioid use and monitoring of opioid use is one of the best ways for providers to know what the patient is doing so that the treatments can be adapted to that patient’s specific situation,” she continues. “But, in addition to information to help us best choose other treatments, the process of monitoring, or paying attention to, what the person is using, is an important first step in treatment itself.”
“Every day there’s news about the opioid crisis,” notes Schmidle. “It’s having widespread effect. The team at CARI Therapeutics is very passionate about making a positive difference for people suffering from substance use disorders, and we strongly believe that technology can play a significant role. This project certainly won’t be the end-all be-all for addressing the opioid crisis, but it could be instrumental in improving the dismal treatment outcomes for people who have opioid use disorders.”
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



