Q&A: Strengthening Antibody Armor for Tripledemic Times
Story by:
Published Date
Article Content
There are many things to look forward to in the coming months, from holiday travel to family gatherings and festive events. Yet the best made plans can be halted by unwelcome guests—viruses that can leave you sneezing, coughing and fatigued.
This season there are three prevalent respiratory viruses to be aware of—influenza, SARS-CoV-2 and respiratory syncytial virus (RSV), all of which are transmitted via aerosols. To learn more about how to protect ourselves and loved ones from these viruses and how vaccination can help, we spoke with Dr. Robert “Chip” Schooley, a professor in the Department of Medicine at UC San Diego School of Medicine and a leader of UC San Diego’s Return to Learn program.
Q. The phrase “tripledemic” has been circulating in the media lately. Which three viruses are involved and what impact could it have?
Schooley: We’re currently experiencing a tripledemic, dominated by SARS-CoV-2 (the virus that causes COVID-19), the influenza (flu) virus and respiratory syncytial virus (RSV). We’re having a lot more flu, and earlier, than last year. We also still have COVID-19 circulating, as well as trouble from RSV—an annual virus that can be harmful for infants, especially those who have cardiac disease or asthma, as well as older adults who have vulnerable lungs from issues like chronic obstructive pulmonary disease (COPD). All three of these viruses are transmitted by aerosols, so masking remains one of the most effective ways to prevent infection.
Q. How can I distinguish between COVID-19, flu and RSV symptoms?
Schooley: At the patient level it’s hard to distinguish between the symptoms. All three can include fever and chills, a cough and runny nose. The flu and COVID-19 viruses also share sore throat, body aches, headache and fatigue.
In the past, COVID-19 could be distinguished by new loss of taste or smell but these symptoms are rare with the currently circulating variants. Nausea, vomiting, diarrhea or shortness of breath can be seen in either flu or COVID-19.
If you have these symptoms, we recommend that you stay home so that there’s no risk of exposing others. Then, complete a COVID-19 test—this can be a home rapid antigen test. Sometimes the rapid antigen test will turn positive very early on when you first begin to feel nasal stuffiness, but sometimes it takes 24 hours or so to turn positive. If it's negative, don't rush out of your home; wait and test yourself again the next day.
Q. What is an “immunity gap” and why has this year presented a change in the typical pattern of viral infections?
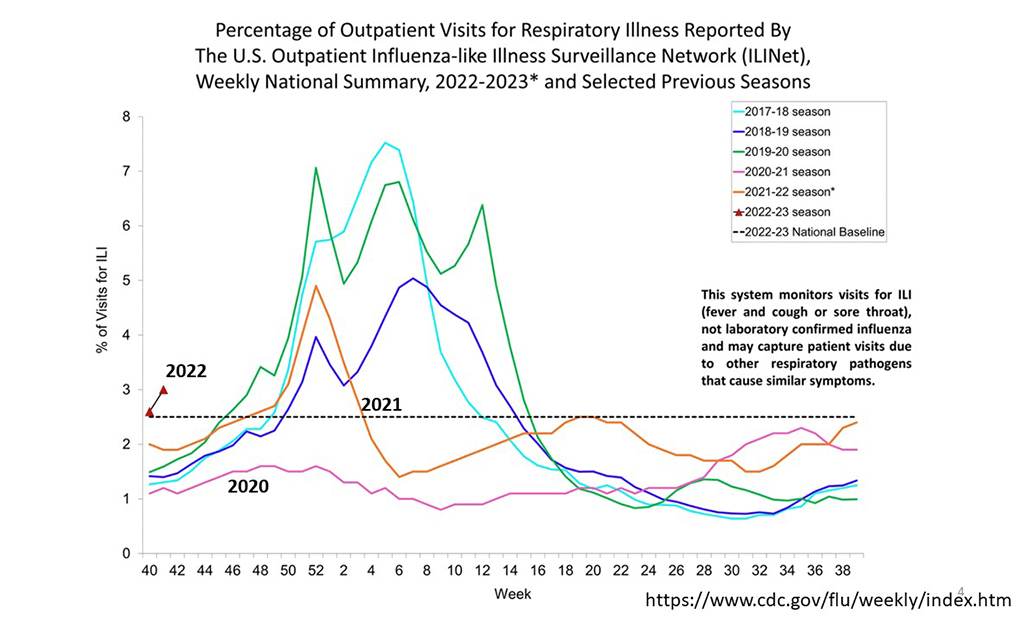
Schooley: Many of us have had a two-year break from infections like influenza and RSV because we have been masking indoors and in public places. During this time, enough of us would typically become infected and we would build immunity at the population level. In the virtual absence of influenza or RSV activity over the past two respiratory virus seasons, our population is much more vulnerable to both viruses. We are already seeing a lot more influenza activity than we have in previous years. The flu typically picks up in the fall and goes through the winter. Prior to the pandemic, infections would start in November and peak in January. However, this year, we are seeing influenza infections spike several weeks early, foreshadowing a strong influenza season.
Q. What is the benefit of getting vaccinated for COVID-19 and the flu?
Schooley: It’s like putting money in the bank for the future. What you're doing is educating your immune system so that when it inevitably runs into the real virus, (either influenza or SARS-CoV-2) it is better prepared to deal with it. Each time your body sees the viral antigen in a vaccine or the virus in an infection, your immune system builds a little more immunity to that virus and goes through a series of maturations that allow more and more sophisticated immune responses in the weeks following. The reasons vaccines work is they are engineered to make the body think it's looking at the real thing. The body doesn't know whether it's looking at the virus or the vaccine, yet it will still make the antibodies that will attack the virus.

Q. Which form of antibodies are most beneficial—the ones that are produced after a COVID-19 infection or the ones that are created after receiving a vaccine?
Schooley: They are both good for you in terms of being able to reduce the chance of getting infected the next time—however, this applies best to those who have received their initial COVID-19 vaccine series. If you don’t have any immunity built up and you’re infected by SARS-CoV-2, you have a good chance of having severe symptoms and a higher chance of experiencing long COVID symptoms and you will build less immunity from that infection than if you had already been vaccinated to “prime” the immune response.
For those who have had their initial vaccination series and experience a breakthrough infection, you gain a big boost in your immunity, similar to receiving a booster shot. Yet even after infection, we still recommend people get a booster shot three months after being sick because this is the time that memory cells are at their peak—circulating the bloodstream on the lookout for any sign of the virus. You will get a very strong antibody boost when they come into contact with what appears to be the virus through vaccination at this point after a round of infection.
The reason we recommend waiting three months isn't because it's dangerous to be vaccinated earlier. You get a much bigger boost of your immunity if you've had a few months for your immune system to mature after the previous experience with it. That’s why when we start out with the original vaccine series, we don't give the first and second shot several days apart.
Q. When is the best time during the fall season to get a flu shot?
Schooley: If you are not busy today, you should go out and get your flu shot—and if the timing is right, your COVID-19 booster as well. You can receive these in the same visit. Influenza vaccines remain strong for six months. It takes two weeks to get to your optimal immunity level, yet the immune system begins to work quickly immediately after the shot. Even if you have a trip planned in a few days, it is still a benefit to get vaccinated now.
Flu shots remain an important form of protection for a virus that can also cause severe disease and hospitalization, particularly for older adults and those who have underlying heart or lung disease. Even healthy people who get the flu can feel pretty terrible for a few days with a high fever.
Q. Why is it necessary to do a 15-minute observation period after receiving a vaccination shot?
Schooley: Some individuals can have an allergic reaction to vaccines, leading to anaphylaxis. This can involve asthma symptoms (airways get tight), or your blood pressure can drop, and you can feel faint. Nurses are on standby to deliver an EpiPen injection; it is rarely fatal but can be frightening for those who experience it. This reaction can happen to many different types of medications, and is caused by an Immunoglobulin E (IgE) antibody in the body that reacts (usually) to something the vaccine is dissolved in.
If someone were going to have such a reaction to a shot, it would happen pretty quickly, and within 15 minutes. We don’t want someone getting a shot and driving home and experiencing this unexpectedly in the car. Sometimes individuals who have a known allergy to a vaccine can be pre-medicated with Benadryl. Those that have a reaction should see an allergist to talk about how to prevent these reactions on the future.
Q. Are there any new COVID-19 strains on the horizon that are concerning?
Schooley: There are three that we're watching closely, and a fourth one that's a little further away. Currently BA.4.6 and BA.5 are the two dominant strains of COVID-19, which began in the summer as Omicron variants. As winter approaches, three new strains are coming to the fore—BQ.1 and BQ.1.1 and BF.7.
One thing that seems to be different is that in the past a new variant would come along and push all the other ones out of the way, only one would dominate. Now we're having several of these variants circulating at the same time. This gives the virus more options because it has a better chance of bumping into somebody who has not yet built immunity against it.
Q. How long are COVID-19 boosters effective?
Schooley: The best protection happens in the first two weeks after getting a vaccine and the following three months. During this period your chances of becoming infected at all are reduced significantly. You are also protected from becoming severely sick and hospitalized. After three months, your chances of getting a breakthrough infection increase but you are still defended from severe symptoms.
How long vaccines remain effective depends on how different the new strain is from the old one, as well as the strength of your immune system. Older adults and those who are immunocompromised may need to get boosted more often, and the more people who receive a vaccine means the less chance the virus can continue to replicate.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.




