Premature Baby Born in 1981 Delivers Premature Twins in 2022 at Same Hospital
Mother receives life-saving care by multi-disciplinary team at UC San Diego Health before and after childbirth
Story by:
Published Date
Story by:
Topics covered:
Share This:
Article Content
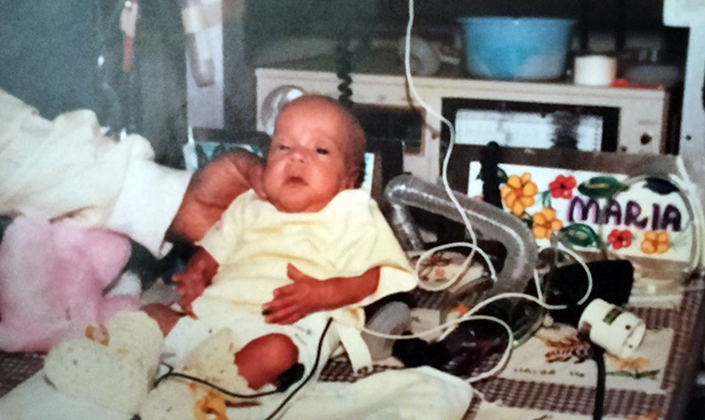
Born at 25 weeks gestation and weighing less than two pounds, Maria “Gabriela” Gastelum spent her first days of life connected to many machines that assisted her underdeveloped organs. Her tiny body faced immense challenges.
The premature birth subsequently led to a severe brain bleed that developed into hydrocephalus, a neurological condition caused by abnormal buildup of cerebrospinal fluid in the cavities deep within the brain.
A few days after she was born, Gastelum was taken into surgery to have a shunt placed in her brain by former UC San Diego Health neurosurgeon Hector James, MD, to help drain cerebrospinal fluid and redirect it to her abdomen where it could be reabsorbed. Shunts help prevent pressure from getting too high in the brain.
It was 1981, and Gastelum was one of the smallest babies at the time to have been cared for in the neonatal intensive care unit (NICU) at UC San Diego Medical Center in Hillcrest.
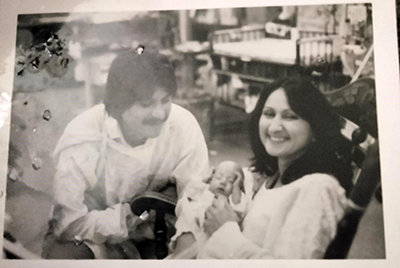
“My parents were determined that I was going to live,” said Gastelum. “I was monitored and received care around-the-clock by a dedicated medical team.”
Linda Levy, RN, MSN, worked at UC San Diego Health for more than 35 years and was the director of Women and Infant Services from 1996 to 2010. She remembers when Gastelum was born.
“She had a very devoted mother,” said Levy. “Throughout my years in health care and at UC San Diego Health, I witnessed how neonatal care evolved and how advancements in technology have allowed more premature babies to survive. It was not until the end of the 1980’s that premature babies born at 25 to 26 weeks gestation survived. Gabriela’s story is remarkable.”
Technology over the past several decades has improved significantly in the NICU setting, from incubators and mechanical ventilators specifically designed for premature infants, monitoring that predicts the risk of life-threatening infections up to 24 hours before they appear and phone apps that allow parents to watch their baby when away from the hospital.
As the region’s only academic medical center, UC San Diego Health treats patients in need of advanced diagnostics and medical and surgical care. The NICU offers complex, specialty care with a multi-disciplinary team, including neonatologists, neonatal nurse practitioners, registered nurses, nutritionists, respiratory therapists and therapists who specialize in occupational and physical therapy.
After six months in UC San Diego Health’s NICU, Gastelum was discharged and able to finally go home.
“It was a huge milestone for me and my family,” said Gastelum. “My parents were so relieved, grateful and overjoyed that I survived and that they could bring me home to start to experience our lives together outside of the hospital setting.”
Taking Steps Forward
As she grew up, Gastelum continued to face challenges from her premature birth that were addressed and treated at a local children’s hospital.
At age 3, she needed her first shunt revision. Experts note that approximately half of all shunts need to be revised or replaced. Throughout the years, Gastelum underwent shunt revisions at UC San Diego Medical Center performed by David Barba, MD, and William Taylor, MD, both neurosurgeons and professors of neurological surgery at UC San Diego School of Medicine.

“Going through shunt replacement is challenging, especially for a young child,” said Gastelum. “Recovery is somewhat difficult. You are sore at the site.”
It was also around this time that it was determined Gastelum had developed cerebral palsy affecting her right side. She underwent multiple orthopedic surgeries to gain strength and mobility.
“I went through years of physical and occupational therapy and learned how to walk in elementary school,” said Gastelum.
And she kept stepping forward from that point on. She graduated college, started a career and got married in 2010.
It was approximately 12 years into their marriage when Gastelum and her husband decided to start another chapter in their lives.
Overwhelmed with Happiness, Times Two
Gastelum and her husband decided they wanted to start a family. She was age 39 at the time and was considered high-risk. She had undergone six shunt and scar revisions, including an abdominal shunt placement that was needed when it was determined the one in her brain had disconnected.

After two years of trying to get pregnant, the couple decided to go through the in vitro fertilization (IVF) process.
“We had a miscarriage on our fifth try. It was heartbreaking,” said Gastelum.
“On our sixth and last try, we got pregnant with twin girls. When I found out the news during the ultrasound, I was overwhelmed with happiness and completely shocked. I called my husband, and he started bawling. We had tried for so long to make our wish of starting a family come true.”
From Almost Comatose to Childbirth
Gastelum’s pregnancy was going well, healthy and on track. She began to receive care with Thomas Moore, MD, professor of in the Department of Obstetrics, Gynecology and Reproductive Sciences at UC San Diego School of Medicine and obstetrician/gynecologist at UC San Diego Health, specializing in high-risk pregnancies.
“When I met with Gabriela and her spouse for the first time at 12 weeks of her pregnancy, she was facing some health issues that put her at high-risk: identical twins, advanced maternal age, history of hypertension and a shunt draining cerebrospinal fluid from her brain into her abdomen area where her babies were growing. All these factors put her at risk of having premature labor and delivery,” said Moore.
“I was endlessly impressed with how the couple maintained great positivity and determination through many prenatal visits and ultrasounds performed to ensure the babies were growing equally and thriving.”
Then 30 weeks into her pregnancy, Gastelum started to feel faint and extremely exhausted.
“I couldn’t even get out of bed for my baby shower,” said Gastelum.
Instead of celebrating the upcoming birth of her twin daughters that day, Gastelum and her husband found themselves in the Emergency Department at UC San Diego Health.
A CT scan showed her ventricles, natural fluid spaces within her brain, were dangerously expanded.
Enter Thomas Beaumont, MD, PhD, assistant professor in the Department of Neurological Surgery at UC San Diego School of Medicine and neurosurgeon at UC San Diego Health.
“Gabriela was very sick and rapidly becoming comatose. We were able to use her existing shunt to quickly remove enough fluid to allow her to wake up. It was like turning on a light switch,” said Beaumont.
However, the shunt failed because the pressure in her abdomen became higher than the normal pressure within her head.
“The existing tube in her brain was then connected to an external collection system outside of her abdominal cavity, and she rapidly recovered,” adds Beaumont. “The challenge was, she was 30 weeks pregnant and would either need the shunt rerouted to her heart, or we would need to keep it externalized until after she gave birth.”
A medical team including neurosurgery, obstetrics, neuro critical care and neonatal intensive care was formed.
“Given the patient’s high risk twin pregnancy, it was our consensus that surgery to place the shunt in her heart would place the babies at risk. We elected to keep Gabriela’s shunt externalized and keep her in the hospital under observation for two weeks until the babies could be safely born by cesarean section,” said Beaumont.
Because of the ongoing maternal and fetal high-risk conditions, Gastelum was closely monitored in the neuro-critical care unit with frequent assessments of the twins’ well-being. The medical team agreed that the twins reaching 32 weeks gestation would significantly reduce the dangers from a premature birth.
“Dr. Moore and Dr. Beaumont are both very attentive and had such good bedside manners,” said Gastelum. “They made me feel like I was in the best hands.”
Entering Parenthood Full Circle
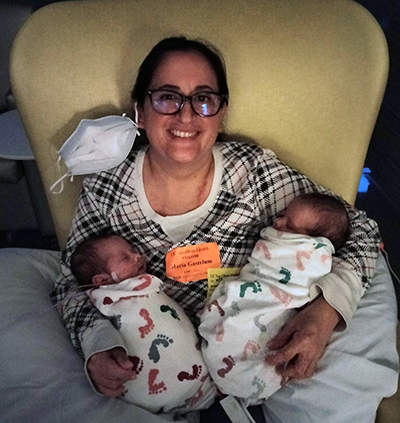
On September 26, 2022, at 32 weeks, Gastelum twins were delivered via planned c-section.
Liyah was born first at 2 pounds and 13.5 ounces, and then one minute later, Natalia was born at 4 pounds and 3 ounces.
“My emotions after giving birth were happiness, relief and amazement. I was so grateful to hear my daughters cry for the first time. It was indescribable. We had waited for so long to hear those cries. My husband and I had tears of pure joy,” said Gastelum.
Like their mom nearly four decades ago, both babies needed care in the NICU. This time, it was at Jacobs Medical Center at UC San Diego Health.
“Our NICU is a nationally recognized center of excellence and our dedicated NICU team provides the highest quality of care to critically ill infants. We put our hearts into our work,” said Jacqueline Iseri, RN, nurse manager of the NICU at UC San Diego health.
“It is rewarding to know we are providing compassionate and advanced care and treatments to our tiniest patients while supporting parents during a vulnerable time. We are honored to be able to get to know families like Gabriela’s and have them entrust us with the care of their precious infants.”
“It is very special to know that the severely premature baby I remember many years ago has now become a parent to beautiful twins and that they all received care from an extraordinary team,” said Levy.
Liyah needed oxygen support and Natalia needed a gastrostomy tube placed for feeding support.
Shortly after the twins’ birth, Gastelum needed her own specialized care — her seventh shunt revision performed by Beaumont and his team.
“We needed to place new shunt tubing into Gabriela’s abdomen and connect it to the valve implanted under the skin on her head. We used a minimally invasive laparoscopic technique with the assistance of Dr. Jula Veerapong in general surgery,” said Beaumont.
“Having gotten to know Gabriela very well during her time in the hospital, we were all delighted to finally repair her shunt and allow her to be disconnected from the external collection system, and most importantly, focus on being a new mother.”

After 107 days in the NICU, both babies were discharged and left the hospital to start a new chapter.
“It felt so good to bring them home. I am very careful about where we go and their exposures due to their vulnerabilities,” said Gastelum.
“I love taking care of them. We are tired and it can be hard, but I am grateful every day. I know we received the best care at UC San Diego Health. It is a true full circle moment, from my own experience and care received as a baby to that of my own babies.”
Both UC San Diego Health hospitals offer NICU support for babies who need special care, including: a Level II Intermediate NICU at UC San Diego Medical Center in Hillcrest for babies who require short-term intensive care after birth, and a Regional Level III NICU at Jacobs Medical Center in La Jolla for babies with critical or more complex medical needs.
“I love taking care of them. We are tired and it can be hard, but I am grateful every day. I know we received the best care at UC San Diego Health. It is a true full circle moment, from my own experience and care received as a baby to that of my own babies.”
Topics covered:
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.




