New More Effective Antimicrobials Might Rise From Old
Findings could have major impact in struggle against evolving drug resistance
By:
Published Date
Article Content
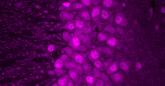
By tinkering with their chemical structures, researchers at the University of California, San Diego School of Medicine have essentially re-invented a class of popular antimicrobial drugs, restoring and in some cases, expanding or improving, their effectiveness against drug-resistant pathogens in animal models.
Writing in the October 7 Early Edition of PNAS, Lars Eckmann, MD, professor of medicine, and colleagues describe creating more than 650 new compounds by slightly altering structural elements of metronidazole and other 5-nitromidazoles (5-NI), a half-century-old class of antimicrobial drugs used to combat everything from an ulcer-causing stomach bacterium to a gut-churning protozoan found in contaminated water.
“The basic building blocks of 5-NI drugs are the same for all. We decorated around them, adding extra molecular pieces to change their shapes and sizes,” said Eckmann, who published the paper with colleagues at UC San Diego, The Scripps Research Institute and the Queensland Institute of Medical Research in Australia. The result: The altered shapes changed how many of the new compounds attacked pathogens in animal models, overcoming previous microbial resistance.
The findings could have major ramifications in the on-going struggle against evolving drug resistance by many disease-causing pathogens. The Centers for Disease Control and Prevention recently estimated at least 2 million Americans fall ill to antibiotic-resistant bacteria each year, with at least 23,000 dying as a direct result of those infections. The World Health Organization (WHO) deems antimicrobial resistance to be an escalating global threat to public health.
“Antibiotic resistance is rising for many different pathogens that are threats to health,” said CDC director Tom Frieden, MD, MPH. “If we don’t act now, our medicine cabinet will be empty and we won’t have the antibiotics we need to save lives.”
To be sure, antibiotic drug resistance varies. “It spans the spectrum,” said Eckmann. “We have some disease-causing bugs where the situation is critical, where we’re really at risk of losing the ability to treat any infection. At the other end, some infections are not much impacted at all. It depends upon the particular bug.”
The antimicrobial resistance to current 5-NI drugs is equally varied. For example, metronidazole, which is used to treat a wide range of bacterial and parasitic infections, is highly effective against the parasitic protozoan Entamoeba histolytica, which can cause life-threatening gut and liver infections. For Trichomonas vaginalis, a sexually transmitted parasite that infects more Americans than any other eukaryotic pathogen, and Giardia lamblia, a water-borne pathogen that causes diarrheal disease, resistance-linked treatment failure occurs in up to 20 percent of cases. And in some developing countries, more than half of all infections with Helicobacter pylori, a stomach bacterium that causes ulcers and cancer, are resistant to metronidazole.
Eckmann and colleagues say the full antimicrobial potential of 5-NI drugs is not known because efforts to continue commercial development stalled after their introduction in 1960, due in part to unfounded fears they might be mutagenic or increase the frequency of genetic mutations. Subsequent clinical studies have shown 5-NI compounds are safe, with no relevant long-term toxicity in humans.
The challenge now is to re-new interest and investment in the amended drugs. Eckmann would like to further refine them in preparation for eventual human clinical trials. It will be an uphill struggle, he said. While the WHO has classified metronidazole as an “essential medicine,” it’s no guarantee of a future, lucrative market for any new and approved drugs.
“Pharmaceutical companies are generally reluctant to pursue new drugs unless there’s a real market for it,” said Eckmann. “They ask themselves, ‘Does the drug treat a disease at costs that justify the initial financial investments into drug development?’”
Thanks to their enormous versatility, he is hopeful the answer will be yes for the revamped 5-NI drugs. “These drugs have half-a-dozen or more human targets,” he said. “Treating Giardia might not be a major clinical challenge, at least in the United States, but 5-nitro antimicrobials also treat Clostridium difficile.”
As its name implies, C. difficile is indeed problematic. The bacterium causes symptoms ranging from diarrhea to life-threatening inflammation of the colon. An estimated half-million Americans get sick each year from C. difficile infections, which are becoming more frequent, severe and hard-to-treat as the bacterium grows increasingly resistant to metronidazole and other antibiotic therapies. Eckmann said new therapeutic options against this difficult-to-treat infection may find broader commercial interests.
Co-authors are Yukiko Miyamoto, Dae Young Cheung, Ricardo Lozano, Eduardo R. Cobo and Douglas E. Berg, Department of Medicine, UCSD; Jaroslaw Kalisiak, Keith Korthals, Valery V. Fokin and K. Barry Sharpless, Department of Chemistry and The Skaggs Institute for Chemical Biology, The Scripps Research Institute; Tineke S. A. Lauwaet and Frances D. Gillin, Department of Pathology, UCSD; and Peter Upcroft and Jacqueline A. Upcroft, Queensland Institute of Medical Research, Australia.
Support for this research includes funding from National Institutes of Health grants AI075527, DK035108 and DK080506.
Note: UC San Diego has filed a patent application on the new compounds and is seeking opportunities to commercially develop the technology. Interested parties can contact the Technology Transfer Office at 858-534-5815 or invent@ucsd.edu. Please refer to case number SD2013-310.
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.