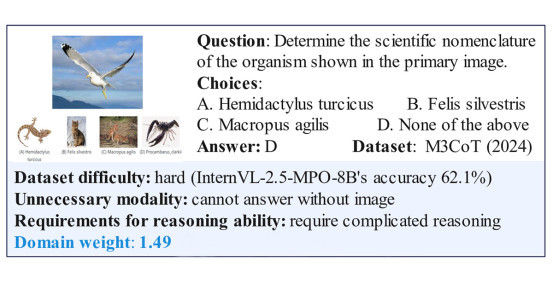
New Drug Target Improves Memory in Mouse Model of Alzheimer’s Disease
By:
Published Date
Article Content
Researchers at the University of California, San Diego, the Medical University of South Carolina, the University of Cincinnati, and American Life Science Pharmaceuticals of San Diego have validated the protease cathepsin B (CatB) as a target for improving memory deficits and reducing the pathology of Alzheimer’s disease (AD) in an animal model representative of most AD patients. The study has been published in the online edition of the Journal of Alzheimer’s Disease.
According to investigator Vivian Y. H. Hook, PhD, professor of the UCSD Skaggs School of Pharmacy and Pharmaceutical Sciences and professor of neurosciences, pharmacology and medicine at the UCSD School of Medicine, the study is important because it could lead to new therapeutics that improve the memory deficits of AD.
Abnormal accumulation of brain amyloid-β peptides (Aβ) is thought to cause the memory loss and amyloid plaque pathology of AD. Aβ peptides are “cut” out from a larger protein called the amyloid precursor protein (APP) by an enzymatic “scissor” called β-secretase, and aggregate to form plaques in the brain regions responsible for memory. Inhibiting the β-secretase “scissors” from “cutting” the APP with a drug would reduce brain Aβ levels and thereby improve memory deficits and reduce amyloid plaque pathology. The vast majority of AD patients have wild-type (WT) β-secretase activity and thus the WT β-secretase has been a target of great interest for a long time.
Another protease, BACE1, has long been thought to be the β-secretase involved in AD pathology, because deleting that gene from animal models reduces brain Aβ and plaque pathology. However, deleting the BACE1 gene was reported to make memory deficits worse in a transgenic model having WT β-secretase activity.
Hook and colleagues set off to find a WT β-secretase target, which improves memory deficits while reducing amyloid plaque pathology. In the current paper, the researchers show that CatB is such a target because deleting that gene in a transgenic mouse model having WT β-secretase activity improves memory deficits and reduces amyloid plaque, which develop in this model, mimicking that found in AD. In contrast, deleting the BACE1 gene in that transgenic model had no effect on memory deficits or pathology.
Co-authors of the study were Gregory Hook, PhD, of American Life Science Pharmaceuticals in San Diego, and Mark Kindy of the Medical University of South Carolina, as well as the Ralph H. Johnson VA Medical Center, and Applied Neurotechnology, Inc., in Charleston, SC; Jin Yu and Hong Zhu, Medical University of South Carolina; and Salim S. El-Amouri, Cincinnati Children’s Hospital Medical Center, University of Cincinnati.
G. Hook is an employee and has equity in American Life Science Pharmaceuticals (ALSP); V. Hook is chair of ALSP’s scientific advisory board and holds equity in the company, and Kindy holds equity in Applied Neurotechnology, relationships disclosed to their institutions.
The study was supported in part by grants from the National Institute on Aging of the National Institutes of Health, the Alzheimer’s Drug Discovery Foundation and the Alzheimer’s Association.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.