Meet us at Phase 0: Inside the HUMANOID™ Center at UC San Diego
By pushing the boundaries of what’s possible in a petri dish, UC San Diego researchers are making drug discovery faster, better and more human
Published Date
Story by:
Topics covered:
Share This:
Article Content
According to physician-scientist Pradipta Ghosh, M.D., the process of getting newly-discovered drugs into the clinic is overdue for a revolution.
This lengthy process begins with years of lab research, often using animal models like mice or fish, to test safety and efficacy. If promising, the drug then enters three phases of clinical trials in humans. Only after succeeding in these trials can the drug be approved by the Food and Drug Administration for widespread use in the clinic. Overall, the process can take more than a decade, and many drugs never make it to the clinic at all.
“Ninety percent of clinical trials for new drugs ultimately fail, and each of these failures comes with a hefty price tag for society,” she said. “This is because trials are both imprecise and expensive, and the current tools we have to test new drugs for safety and efficacy simply aren’t up to the task.”

To Ghosh, the problem with the early testing phases of drug discovery, before a drug enters clinical trials, can be summarized succinctly.
“We are not mice.”
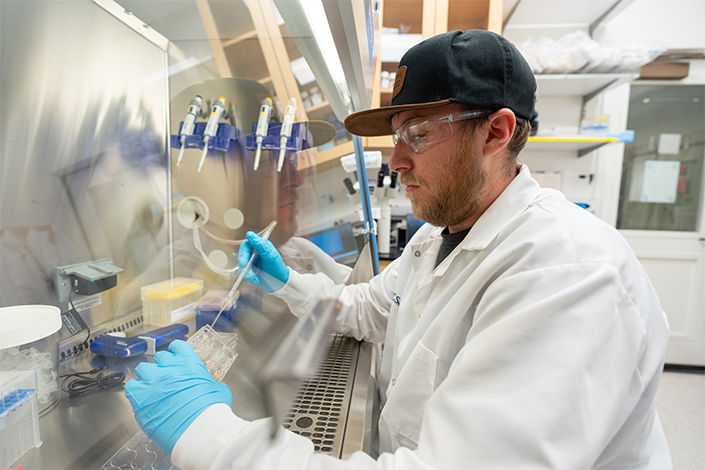
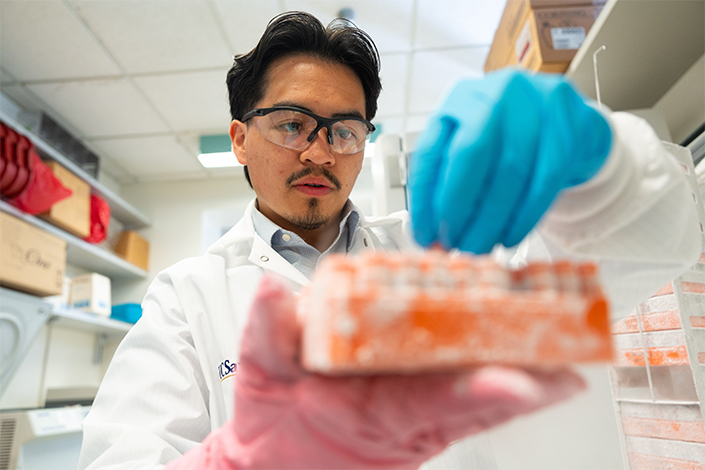
Ghosh is at the helm of the HUMANOID™ Center for Excellence at the University of California San Diego, which is pioneering the use of patient-derived-organoids — miniature, three-dimensional models of human organs grown from a patient’s cells. Many scientists utilize organoids that are grown from donor cells, such as from skin or blood, that have been reprogrammed to grow into a certain type of tissue, such as brain tissue. However, HUMANOID™ takes a different approach entirely.
By growing their organoids from real patients’ cells, taken directly from the organ system they are seeking to replicate, they can make organoids that more accurately represent the diseased organ of a specific patient. The result is a more precise and relevant testing ground for new drugs and other treatments.
Their tagline “Meet us at phase zero,” refers to their goal of streamlining the process of getting new drugs—that are safer and more effective—into clinical trials.
“HUMANOID™ was founded at a time when the world had yet to recognize the full potential of stem-cell based human models in biomedical research, and nobody thought it could be possible to bypass animal models in drug discovery research,” said Ghosh, professor of cellular and molecular medicine at UC San Diego School of Medicine. “We hit a lot of resistance in the beginning, but today, HUMANOID™ stands as a model for how to launch transformative, high-risk, high-reward research enterprises at scale, even in uncertain times.”
A paradigm shift
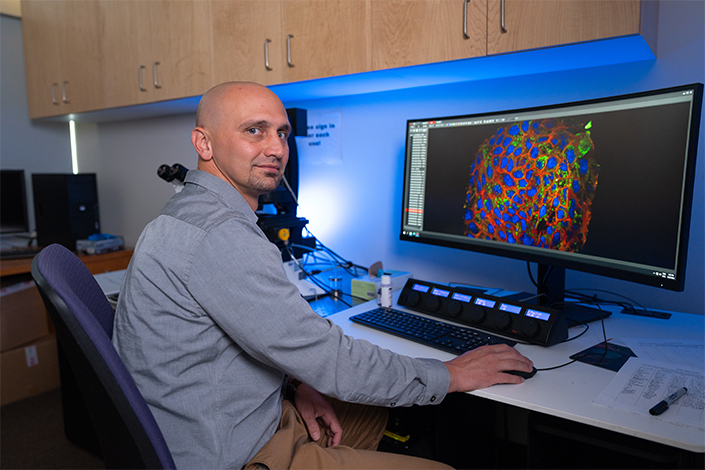
To create organoid models of disease, HUMANOID™ relies upon engineering principles, utilizing precise mathematical equations to identify the drivers of human diseases from wide pools of patient data. This allows them to create organoids that accurately and precisely replicate the drivers of disease.

“We at HUMANOID™ wanted to bring mathematical precision into organoid models,” said Ghosh. “This is because math is expected to yield consistent results that can be reproduced. The answer today will be the same tomorrow as it will be a year from now. If an imprecise process like drug discovery requires precision, there is no better place to bet on than math!”
Their innovative approach has already yielded several breakthroughs. During the COVID-19 pandemic, HUMANOID™ developed the first-ever organoid model of a complete human adult lung, which helped scientists understand why adults are much more likely to develop severe lung symptoms than children. Their model also helped identify new therapeutic targets for long-term complications of COVID, such as lung scarring. They’re now continuing to utilize math-assisted identification of disease drivers to reveal the potential of new drugs to halt and reverse these complications.
The HUMANOID™ approach is not, however, limited to any one tissue area or organ system. Most recently, their approach has also yielded a new way to provide therapies tailored to patients suffering from inflammatory bowel diseases, a complex debilitating inflammatory condition of the gut that impacts people of all ages. They also discovered a method to reprogram cancer stem cells, a subgroup of cancer cells that are thought to be responsible for the initiation and progression of cancers. Cancer stem cells are also thought to be the reason cancer is often able to evade treatment.
Their reprogramming process prompts cancer stem cells to revert into normal, healthy stem cells. If this process fails, the cancer stem cells ultimately die, leaving healthy stem cells unscathed. Ongoing research at HUMANOID™ is revealing that this form of treatment could impact a wide range of cancers because it targets a mathematically pinpointed driver of cancer, regardless of the location or type of cancer.
“This discovery represents a paradigm shift in our ability to neutralize—at its root—cancer’s indomitable spirit to spread, resist treatment, relapse, and kill,” said Ghosh.
In addition to a lab generating new discoveries, HUMANOID™ is also a service hub, providing organoid research support for scientists and industry partners around the world. One of the center’s most ambitious service initiatives is their organoid biobank — a collection of organoids from different tissues, diseases, and patients, which are available to researchers for use in their own experiments.
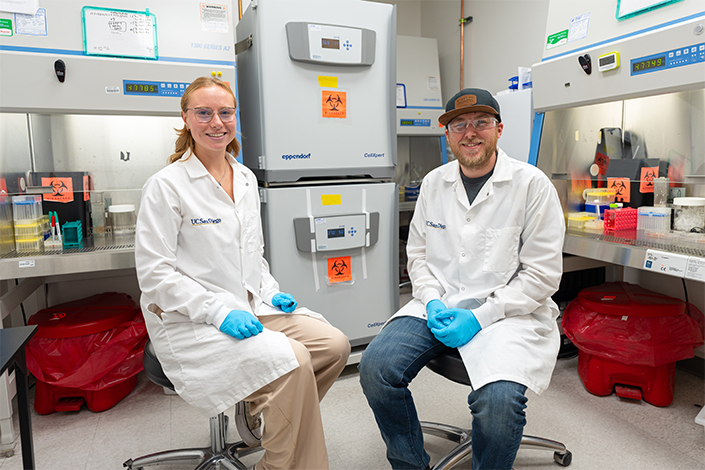
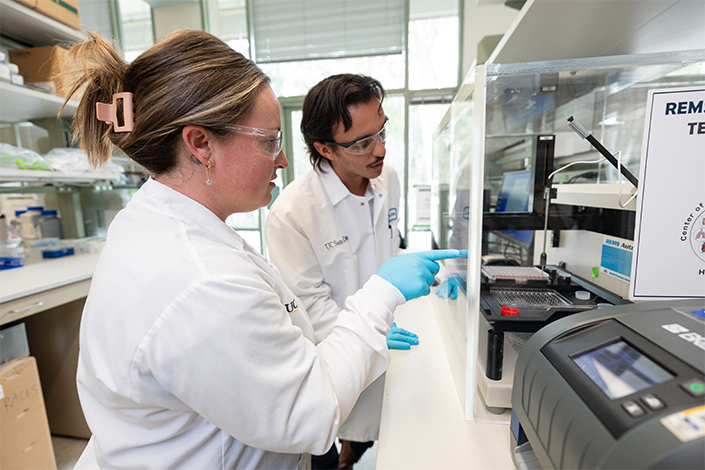
“HUMANOID™ is a complex research initiative—much more than my own laboratory,” added Ghosh. “The responsibility of working with patient-derived models is one we carry with humility and purpose. My job is easy when I am surrounded by people willing to walk into the unknown, just out of curiosity, a shared purpose of service, and a deep commitment to giving back. Led by its fearless director, Courtney Tindle, HUMANOID’s scientists bring this vision to life.”
The engine of progress
While HUMANOID™ has grown quickly, the center’s progress could come under threat due to proposed cuts to National Institutes of Health (NIH) funding, which has supported Ghosh’s own research programs for more than a decade and has been instrumental in helping HUMANOID™ take off.
The proposed cuts could have a significant impact on HUMANOID’s future research. In addition to directly funding research projects, the NIH also funds the indirect costs of research, such as maintaining facilities and equipment. NIH funding also helps cover administrative costs, including human resources, regulatory oversight, and grant management.
“HUMANOID™ is not just a lab — it’s an entire ecosystem of research and service,” said Ghosh. “Indirect costs are the invisible yet vital infrastructure that keeps that ecosystem alive. Without them, the entire system would slowly break down.”
The consequences of such cuts would, according to Ghosh, ripple far beyond the walls of the HUMANOID™ center, or even the bounds of the UC San Diego campus.
“Science is the engine of progress, driving discoveries that transform health, technology, and the very fabric of our society. A world with less science is a world with fewer answers, fewer cures, and fewer opportunities to harness the full potential of human ingenuity.”
Or, more pointedly:
“A reduction in science funding is not just a setback for researchers, it’s a setback for all of humanity."
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.





