Accessible and Affordable Care at Heart of Healthcare Technology Grants
Winners receive up to $100K to commercialize innovations
By:
- Catherine Hockmuth
Published Date
By:
- Catherine Hockmuth
Share This:
Article Content

With the proposed technology, the physician can review, revise, and approve a new treatment plan using a smart phone to interact with the GPU cloud. Photo Credit: Steve Jiang, UC San Diego Moores Cancer Center.
Five teams of scientists from multiple campuses of the University of California and a Southern California hospital have been awarded up to $100,000 each to commercialize their ideas for new, lower cost health care technologies that will address a long-standing need for more affordable and efficient chronic disease management and preventive health care, particularly in underserved communities. The commercialization grant program is led by the von Liebig Entrepreneurism Center at UC San Diego Jacobs School of Engineering.
Chosen from a field of 64 applicants from 10 different institutions in Southern California, the projects range from smart phone-based disease diagnostics and weight-loss management tools to a device that turns cell phones into microscopes. Selected university-based engineers, physicians and entrepreneurs will now work with von Liebig technology and business advisors on prototype development and testing, proof-of-concept studies. MBA students from the UC San Diego Rady School of Management will provide support to the innovator teams in the form of market research and competitive analysis.
The awards are part of the von Liebig Center’s Southern California Healthcare Technology Acceleration Program, which nurtures and accelerates the commercialization of novel healthcare inventions developed within research institutes and universities in Southern California.
The program is sponsored by the California HealthCare Foundation, Booz Allen Hamilton, and the Pioneer Portfolio of the Robert Wood Johnson Foundation. A project’s success will be determined by the ability to secure follow-on funding for further development after the initial grant period.
“The California HealthCare Foundation is eager to spark innovations that can reduce the costs of health care and expand access to services for the underserved,” said Veenu Aulakh, a Senior Program Officer at the Oakland-based foundation. “Sometimes great concepts need nurturing at the early stages, allowing them to prove their effectiveness and garner sustained support.”
About the winners:
Steve Jiang, PhD and Yuanyuan Zhou, PhD, University of California, San Diego (UCSD) Departments of Radiation Oncology and Computer Science and Engineering:
GPU and Cloud-based Next Generation Cancer Radiotherapy Treatment Planning
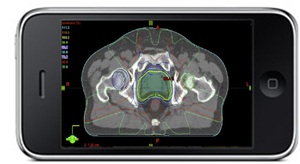
Approximately two-thirds of U.S. cancer patients are treated with radiotherapy because it has proven a particularly effective treatment for many cancer types. The main objective of radiotherapy is to deliver a lethal dose of radiation to the tumor to kill cancerous cells while sparing surrounding healthy organs and normal tissues. The treatment is complex and very patient-specific and must be carefully inspected and approved by the attending physician. Unfortunately, until now, this has meant using a dedicated computer and software system for treatment planning that is expensive and lengthy, often taking as long as one to two weeks to develop and approve. Treatment data may also be stored in individual institutions and different formats, which is costly to maintain and difficult to share among institutions.
This UC San Diego research team is developing a next-generation, web-based treatment planning system that promises to reduce the cost of treatment planning, make better use of physician time, encourage treatment data sharing and improve the effectiveness of radiotherapy devices. Jiang is a professor and executive director of the Center for Advanced Radiotherapy Technologies in the Department of Radiation Oncology at the UC San Diego Moores Cancer Center. Zhou is a professor in the Department of Computer Science and Engineering and Qualcomm Chair in Mobile Computing at the UC San Diego Jacobs School of Engineering. Their system combines graphics processing unit (GPU) technology, which was developed for high-resolution graphics in video games and has become popular for high-performance scientific computing, with cloud computing, through which computation and data storage are provided through a third-party Internet service. Hospitals would simply pay a fee for processing each plan, eliminating any need to maintain their own in-house treatment planning systems. In the proposed system, GPU would be used to design optimal treatment plans through cloud computing. The resulting treatment plan would be delivered to the physician via any small mobile device such as a smart phone. Their research partnership combines Zhou’s expertise in cloud computing with Jiang’s expertise in medicine, and, in particular the role of GPU in medicine, bringing the latest advances in computer science to bear on a significant medical problem.
Aydogan Ozcan, PhD, UCLA Departments of Electrical Engineering and Bioengineering:
Microscopy on a Cell-phone as a Diagnostic Tool (LUCAS)
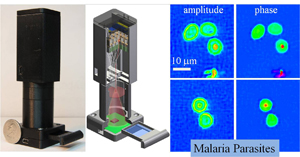
(L) The lens-free super-resolution microscope can be attached to a cellphone or a laptop using a USB cable. (R) Super-resolution microscope shows the signatures of malaria parasites in red blood cells. Photo Credit: Aydogan Ozcan at UCLA Engineering.
This UCLA group has pioneered a lens-free, on-chip imaging modality termed LUCAS, which enables converting conventional cell phones into microscopes and diagnostic tools, providing an important solution to various rural and inner city medicine needs. The first application for LUCAS is the Complete Blood Count (CBC), a broad diagnostic blood test that alerts doctors to a wide range of disorders including anemia, infection and poor nutrition, major problems affecting young children in poor communities. CBC is a critical laboratory test for aid in diagnosis and management of these conditions, and one of the most widely ordered laboratory tests in medicine.
Morbidity and mortality are disproportionally high in children from resource poor settings and disenfranchised populations particularly those living in rural or inner city areas of the United States. Poverty, limited access to health care, poor nutrition, and low level of parental education all contribute to these troubling statistics.
With instant availability of CBC results, physicians, physician assistants, or nurse practitioners will be in a better position to make a diagnosis and prescribe the right drugs during an initial patient contact that can take place practically anywhere. Being able to diagnose and prescribe medicine in one visit also reduces the need for follow-up appointments, which patients in poor communities frequently miss. The platform can also be used, through telemedicine, to guide referral to other medical services. And, by doing tests in-house rather than sending the blood specimens to outside labs, the provider can capture significant additional value for themselves or their institution. This is of particular importance for many organizations that are chronically underfunded and dependent upon government or philanthropic agencies.
Chi On Chui, Ph.D., University of California, Los Angeles (UCLA), Department of Electrical Engineering:
Low-Cost Semiconductor Test Strips for Accurate In Vitro Diagnostics
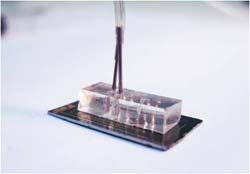
A disposable semiconductor test strip prototype for in vitro diagnostics. Photo Credit: Chi On Chui at UCLA Engineering.
This project seeks to exploit a low-cost, nanoengineered sensor technology for rapid, point-of-care diagnosis of acute diseases in critical settings such as emergency rooms, intensive care, ambulances and even your doctor’s office. For example, evidence of long-term cardiac injury appears early in blood samples, but often in very low concentrations immediately following a heart attack. The researcher has completed a proof-of-concept study of the sensor technology showing that it is 10 times more sensitive than the leading nanoelectronic sensors and provides results in minutes, making it easier for health care providers to recognize and treat cardiac injury. This platform technology will be packaged in a simple hand-held reader interfaced with a disposable test strip, and will ultimately be applied to other disease diagnostics in point-of-care scenarios where ease of use, fast results and low cost are critical for adoption, especially in areas where healthcare resources are inadequate.
Michael Miyamoto, MD, University of California, Irvine (UCI) and Mission Hospital:
Integrated Heart Failure Disease Management

Dr. Michael Miyamoto, UC Irvine Healthcare Executive MBA grad student and cardiologist at Mission Hospital, is developing a disease management system that makes it easier for doctors to monitor patients remotely.
Heart disease patients require long-term, outpatient monitoring to maintain their health and prevent problems that can land them back in the hospital. Unfortunately, current chronic disease monitoring systems for heart failure (HF) aren’t achieving this goal. According to hospital admission data, HF patients have a 25 to 30 percent readmission rate in the first 30 days following discharge. Miyamoto has developed a disease management system that combines necessary clinical monitoring with a user-friendly device that allows doctors to receive regular, wireless updates about the condition of their patients such as whether they are accumulating fluid in their chest, a common indicator that the heart is deteriorating. While the entire potential market for the technology is made up of all patients discharged after a HF hospitalization, implementation of the technology could be focused on patients doctors believe are most at risk for readmission. The economic burden of HF care upon the health care system exceeds $40 billion annually with impatient care comprising the bulk of this cost at just under $30 billion, according to recent data from the American Heart Association. Given the mounting fiscal challenges faced by Medicare and other payers, there is significant opportunity to address the unmet needs inherent in the existing systems of management of chronic disease. Effective monitoring of HF patients will reduce the number of hospital readmissions and expenses to Medicare and other payers.
Michael Leon, PhD, University of California, Irvine (UCI) Department of Neurobiology & Behavior:
Mobile Mandometer® for At-Home Weight Normalization

The Mandometer's small scale and monitoring system provides feedback on eating behavior, training patients how to normalize their eating pattern and eat less without feeling hungry. Photo Credit: Jenny Nolstam, The Mando Group.
“Obesity is the century’s greatest public health threat,” according to the 2010 Dietary Guidelines for Americans report released by the U.S. departments of Agriculture and Health and Human Services. Indeed, Americans spent about $60 billion last year in largely unsuccessful attempts to lose weight and they also lost an estimated $73 billion in productivity to obesity. Obesity also raises the risk for diabetes, glaucoma, kidney damage, cardiovascular and other diseases, which add additional billions of dollars each year to U.S. medical costs.
The Mando Group has demonstrated the effectiveness of a treatment that trains obese patients (including children and teens) to normalize their food intake by providing real-time feedback about eating behavior during and between meals through a device called a Mandometer (mando means “I eat” in Latin). The Mandometer consists of a small scale that sits under a dinner plate that sends information about their eating behavior to a small monitor, which also shows the eating behavior of a normal-weight person to allow patients to model it. Such training allows them to normalize their eating pattern and thereby eat less without feeling hungry.
Having shown the device’s effectiveness, the Mando Group is working to move it out of a clinical setting by developing a more affordable, portable device that can communicate wirelessly with smart phones. They will use the power of the iPhone and Android operating systems to develop a portable scale and three smart phone applications that will help patients recognize fullness during a meal, hunger between meals and provide a virtual therapist for additional practical support needed for an effective weight-loss program away from the clinic.
About the Program
"This program is an effective way to inspire our scientists and engineers in our great universities to focus on developing solutions to real world problems. That, in turn will lead to the creation of great products and companies that will set the foundation for job creation,” said Rosibel Ochoa, executive director of the von Liebig Entrepreneurism Center at UC San Diego Jacobs School of Engineering. “We are excited to provide technology acceleration programs that meet the needs of our partners, students and society.”
The current competition was aimed at supporting the development of early-stage innovations toward commercially viable products or services involving non-pharmaceutical therapies, medical diagnostics and devices. To be considered, the candidate projects were required to have a focus on lowering health care system costs with technologies or services that:
- are significantly less expensive than the current approach, or
- provide care in a lower-cost setting, such as an outpatient clinic, or
- make more efficient use of skilled healthcare professionals
“Booz Allen Hamilton understands the power of new, innovative ideas to create change in the healthcare industry,” said Timi Leslie, vice president, Booz Allen Hamilton. “Programs like this provide the needed platform to identify and nurture the solutions of the future. Booz Allen Hamilton is proud to be a sponsor and participate in selecting the winning ideas.”
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.