Critical Questions
Researchers study human milk, pregnancy and COVID-19.
Published Date
Story by:
Share This:
Article Content
When the global pandemic hit in March 2020, there was great uncertainty for lactating and pregnant parents: Is COVID-19 transmitted via human milk? Can human milk protect infants from COVID-19? Researchers at University of California San Diego School of Medicine immediately started looking for answers. “On one hand, we already know human milk protects the baby from many diseases, such as diarrhea and pulmonary infections. But we also know that human milk can be a vehicle for some diseases to spread in the milk to the baby,” says Lars Bode, PhD, founding director of UC San Diego’s Larsson-Rosenquist Foundation Mother-Milk-Infant Center of Research Excellence (MOMI CORE).
“We knew that pregnant and lactating parents were contracting COVID-19, but the fact of the matter was that we knew very little about its short- and long-term effects on a developing baby,” says Christina Chambers, PhD, MPH, director of the Organization of Teratology Information Specialists (OTIS) MotherToBaby Pregnancy Studies and UC San Diego’s Mommy’s Milk Human Milk Research Biorepository.
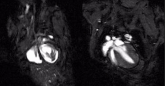
For the COVID-19 and human milk study, the Human Milk Research Biorepository recruited residents of the United States or Canada, who were currently lactating and had tested positive for the COVID-19 virus.
Parents were interviewed by telephone, provided one or more milk samples, and were asked to release relevant medical records from their health care providers.
Together, with collaborators at University of California Los Angeles, it took the team 161 days from the beginning of the pandemic to publish their results that human milk is unlikely to be a source of active virus and does not pose a harm to the human milk-fed baby.
“Under normal circumstances, 161 days from study conception to peer-reviewed publication would be considered extraordinarily fast, but for a crisis like this, it means 161 days of uncertainty for parents, health care providers, and public health authorities,” says Bode.
As COVID-19 vaccines became available, another challenge arose. The vaccines had not been tested in pregnant or lactating parents, which raised new concerns: For example, are the COVID-19 vaccines, and mRNA vaccines in particular, safe for pregnant and lactating parents and their babies? Can these vaccines potentially not only protect these parents, but also their babies?
“In the first few days, not knowing the answers to these fundamental questions led to families choosing between vaccination and human milk feeding their child,” says Bode.
MotherToBaby was tapped by the Centers for Disease Control and Prevention as the trusted resource for the public to answer questions about the safety of COVID-19 vaccines in pregnancy and lactation.
“With a large influx of families contacting MotherToBaby and wanting to help find answers, we were quickly able to use our existing pregnancy and lactation study protocols to address the new research questions about the safety of vaccines,” says Chambers.
Over the course of the next 18 months, MotherToBaby pregnancy studies recruited more than 2,000 people across the U.S. and Canada who had been vaccinated with one or more doses of a COVID-19 vaccine during pregnancy. The study continues to collect outcome information for parents and infants through the one-year post-partum period.
Over the same period, the Human Milk Research Biorepository recruited more than 1,200 lactating parents who had been vaccinated against SARSCoV-2, obtained information about vaccine-related side-effects and collected serial milk samples before, during and after vaccination.
“We found a similar side-effect profile in parents who were vaccinated compared to the general population, and we found no evidence of serious adverse events in the infants who were being human milk fed,” says Chambers.
Additional analyses of these data are ongoing and expected to be published later this year.
“We will continue to address the benefits and safety of COVID-19 vaccinations, booster doses and new vaccine formulations, as well as new antivirals and other new treatments during pregnancy and lactation,” says Chambers.
The group is exploring strategies to create a ‘Public Health Surveillance & Rapid Response Team’ that builds on the unique human milk expertise at UC San Diego and combines it with the university’s new PREPARE Institute. The entity will develop response protocols that can be activated as soon as the next pandemic or other environmental threat emerges.
“Next time, we will be even faster in determining if human milk and novel vaccines or other therapeutics are safe and potentially even beneficial for the baby,” says Bode. “We had the right expertise and collaborators at hand when COVID-19 hit, but we won’t always be this lucky if we don’t learn from this pandemic and put a structured response plan in place.”
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.