Body’s Own Gene Editing System Generates Leukemia Stem Cells
Inhibiting the editing enzyme may provide a new therapeutic approach for blood cancers
Published Date
Article Content
Cancer stem cells are like zombies — even after a tumor is destroyed, they can keep coming back. These cells have an unlimited capacity to regenerate themselves, making more cancer stem cells and more tumors. Researchers at University of California San Diego School of Medicine have now unraveled how pre-leukemic white blood cell precursors become leukemia stem cells. The study, published June 9 in Cell Stem Cell, used human cells to define the RNA editing enzyme ADAR1’s role in leukemia, and find a way to stop it.
While DNA is like the architect’s blueprint for a cell, RNA is the like the engineer’s interpretation of the blueprint. That RNA version is frequently flawed in cancer. While many studies have uncovered pivotal DNA mutations in cancer, few have addressed the roles of RNA and mechanisms that regulate RNA.
“In this study, we showed that cancer stem cells co-opt a RNA editing system to clone themselves. What’s more, we found a method to dial it down,” said senior author Catriona Jamieson, MD, PhD, associate professor of medicine and chief of the Division of Regenerative Medicine at UC San Diego School of Medicine.
The enzyme at the center of this study, ADAR1, can edit the sequence of microRNAs, small pieces of genetic material. By swapping out just one microRNA building block for another, ADAR1 alters the carefully orchestrated system cells use to control which genes are turned on or off at which times.
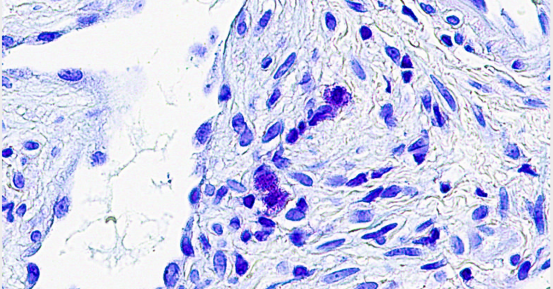
ADAR1 is known to promote cancer progression and resistance to therapy. In this study, Jamieson’s team used human blast crisis chronic myeloid leukemia cells in the lab, and mice transplanted with these cells, to determine ADAR1’s role in governing leukemia stem cells.
The researchers uncovered a series of molecular events. First, white blood cells with a leukemia-promoting gene mutation become more sensitive to signs of inflammation. That inflammatory response activates ADAR1. Then, hyper-ADAR1 editing slows down the microRNAs known as let-7. Ultimately, this activity increases cellular regeneration, or self-renewal, turning white blood cell precursors into leukemia stem cells. Leukemia stem cells promote an aggressive, therapy-resistant form of the disease called blast crisis.
“This is the first mechanistic link between pro-cancer inflammatory signals and RNA editing-driven reprogramming of precursor cells into leukemia stem cells,” said Jamieson, who is also deputy director of the Sanford Stem Cell Clinical Center at UC San Diego Health, director of the CIRM Alpha Stem Cell Clinic at UC San Diego School of Medicine and director of stem cell research at UC San Diego Moores Cancer Center.
After learning how the ADAR1 system works, Jamieson’s team looked for a way to stop it. By inhibiting sensitivity to inflammation or inhibiting ADAR1 with a small molecule tool compound, the researchers were able to counter ADAR1’s effect on leukemia stem cell self-renewal and restore let-7. Self-renewal of blast crisis chronic myeloid leukemia cells was reduced by approximately 40 percent when treated with the small molecule, called 8-Aza, as compared to untreated cells.
“Based on this research, we believe that detecting ADAR1 activity will be important for predicting cancer progression. In addition, inhibiting this enzyme represents a unique therapeutic vulnerability in cancer stem cells with active inflammatory signaling that may respond to pharmacologic inhibitors of inflammation sensitivity or selective ADAR1 inhibitors that are currently being developed,” Jamieson said.
Study co-authors include: Maria Anna Zipeto, Angela C. Court, Anil Sadarangani, Nathaniel P. Delos-Santos, Larisa Balaian, Gabriel Pineda, Sheldon R. Morris, Cayla N. Mason, Ifat Geron, Christian Barrett, Daniel J. Goff, Russell Wall, Kelly A. Frazer, Leslie A. Crews, Qingfei Jiang, UC San Diego; Hye-Jung Chun, Marco A. Marra, BC Cancer Agency; Maurizio Pellecchia, Sanford Burnham Prebys Medical Discovery Institute; and Mark Minden, Princess Margaret Hospital.
This research was funded, in part, by the National Institutes of Health (5K12GM068524, 2P30CA023100-28, R21CA189705), CIRM (RN2-00910-1, DR1-01430, RS1-00228-1), Canadian Institute of Health Research, Office of the Assistant Secretary of Defense for Health Affairs - Peer Reviewed Cancer Research Program, Genome Canada and Ontario Genomics Institute, Moores Family Foundation, Sanford Stem Cell Clinical Center, San Diego Foundation, Ratner Family Foundation and Mizrahi Family Foundation.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.