Biologists Uncover Mechanisms for Cholera Toxin’s Deadly Effects
By:
- Kim McDonald
Published Date
By:
- Kim McDonald
Share This:
Article Content
Biologists at the University of California, San Diego have identified an underlying biochemical mechanism that helps make cholera toxin so deadly, often resulting in life-threating diarrhea that causes people to lose as much as half of their body fluids in a single day.
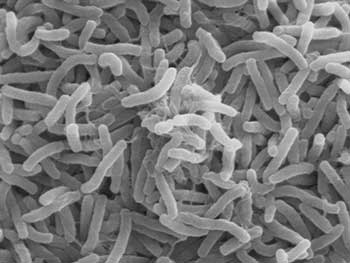
Cholera toxin is produced by the highly infectious bacterium Vibrio cholerae. Credit: Wikipedia Commons
Two groups of scientists working on fruit flies, mice and cultured human intestinal cells studied cholera toxin, produced by the highly infectious bacterium Vibrio cholerae. They discovered the toxin exerts some of its devastating effects by reducing the delivery of proteins to molecular junctions that normally act like Velcro to hold intestinal cells together in the outer lining of the gut.
Their findings, published in the September 11 issue of the journal Cell Host & Microbe, could guide the development of new therapies against the deadly disease, which threatens millions of people in poor countries around the world who live in areas with poor sanitation, with water supplies frequently contaminated by the cholera bacterium. The worst cholera epidemic in recent history occurred after the 2010 earthquake in Haiti, killing more than 7,900 people and hospitalizing hundreds of thousands in Haiti and in the neighboring Dominican Republic.
“We uncovered a mechanism by which cholera toxin disrupts junctions that normally zip intestinal epithelial cells together into a tight sheet, which acts as a barrier between the body and intestinal content,” said Ethan Bier, a professor of biology at UC San Diego who headed one of the two teams. “A consequence of these weakened cell junctions is that sodium ions and water can escape between cells and empty into the gut.”
The study built on research published decades ago, when scientists discovered that cholera toxin caused the overproduction of small chemical messenger molecule, cyclic adenosine monophosphate, or “cAMP,” in epithelial cells lining the intestine.
“High levels of cAMP activate a protein channel called CFTR that allows the negatively-charged chloride ions to rush out of intestinal epithelial cells into the contents of the gut,” said Victor Nizet, MD, a professor of pediatrics and pharmacy at UC San Diego School of Medicine, who headed the other team. “Through basic physiological principals known as electroneutrality and osmotic balance, these secreted chloride ions must be accompanied by positively-charged sodium ions and water, altogether leading to a profuse loss of salt and water in the diarrheal stools.”

The worst cholera epidemic in recent history occurred after the 2010 earthquake in Haiti, killing more than 7,900 people. Credit: Wikipedia Commons
The molecular mechanism by which this massive flux of sodium and water into the gut occurs as a result of the cholera toxin remained a mystery until Annabel Guichard—a research scientist working in Bier’s laboratory and the lead author of the paper—began conducting experiments that spearheaded the two groups’ collaboration.
The UC San Diego researchers found that cholera toxin acts by two entirely distinct, but cooperating mechanisms to produce diarrhea. In addition to increasing the efflux of chloride ions through the CFTR channel, it weakens cell junctions to allow a rapid outflow of counterbalancing sodium ions and water between the cells. The scientists showed that many of the effects of the cholera toxin on the gut could be reversed by genetic manipulations that bolster the delivery of proteins to these junctions.
Understanding this novel mechanism of cholera action could also have important implications for other disorders of intestinal barrier function such as Crohn’s disease, colitis and celiac disease.
“The development of drugs that mimic the genetic manipulations performed in our study may help restore integrity to a damaged intestinal barrier,” said Guichard. “This new approach could reduce disease symptoms in cholera and other chronic gut disorders.”
Other co-authors of the paper include Beatriz Cruz-Moreno, Berenice Aguilar, Nina van Sorge, Jennifer Kuang, Adrianne Kurkciyan, Guillaume P. Pineton de Chambrun and Declan McCole of UC San Diego; and Zhipeng Wang, Saiyu Hang and Paula Watnick of Children’s Hospital in Boston. Funding for the study was provided by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (AI070654 and AI057153).
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



