An HIV Prevention Pill for Transgender Persons
UC launches first in the nation demonstration project; UC San Diego School of Medicine part of effort
Published Date
By:
- Scott LaFee
- Lisa Loeb Stanga
Share This:
Article Content
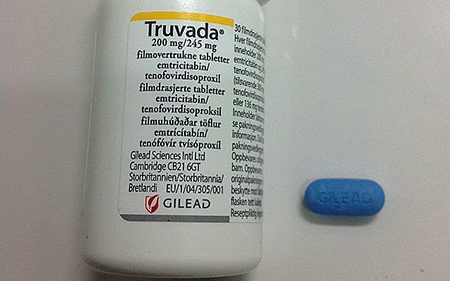
UC launches the first PrEP demonstration project in the United States to focus exclusively on transgender persons. Photo courtesy of Wikimedia Commons
The California HIV/AIDS Research Program (CHRP) of University of California has awarded grants totaling $9.4 million to three teams of investigators to provide and evaluate PrEP – the HIV prevention pill – among transgender persons at risk for HIV acquisition in California.
It is the first PrEP (pre-exposure prophylaxis) demonstration project in the United States to focus exclusively on transgender persons.
Three research teams – one in San Diego and Los Angeles and two in the San Francisco Bay Area – will offer PrEP to an estimated 700 transgender women and men, with a special focus on transgender persons of color, over the next four years. Researchers will design and implement novel, targeted interventions to increase access, uptake and adherence in the transgender community. As part of this work, the research team will also investigate potential drug interactions between PrEP and hormone use.
Transgender persons are extremely vulnerable to HIV infection. By some estimates, transgender women are up to 50 times more likely to be infected with HIV compared with other adults. Efforts are needed to deliver effective prevention services to this population.
Transgender persons of color have been particularly impacted by HIV. While previous PrEP demonstration projects have focused on men who have sex with men, data on PrEP use and implementation within the transgender community is scant.
Transgender populations face a number of HIV prevention challenges, including sociocultural, economic and health-related factors. Some of the barriers include stigma and transphobia, lack of protections against discrimination, trauma, violence, substance use and poor mental health, sex work, incarceration, homelessness, unemployment and limited access to trans-friendly health care. While some work has been done to address these challenges, experts say more is needed, including efforts that not only tackle these underlying drivers of risk but that also employ recent advances in the biomedical prevention of HIV.
Limited research suggests that compared to cisgender men (men assigned male sex at birth and who also identify as male), transgender persons taking PrEP may face additional barriers to adherence, especially for those who are most at risk of acquiring HIV. For example, transwomen have expressed concerns about potential interactions between PrEP and hormone therapy, which could impact adherence.
While drug interactions are not expected between these medications, confirmation is important. By launching this first-of-its-kind PrEP demonstration project, CHRP will help to address barriers to PrEP in the transgender population. “These studies will provide critical information on the implementation of PrEP among transgender people in California, and will help guide state and national efforts to address the epidemic in this often neglected population at high risk for HIV,” said George Lemp, DrPH, director of the UC-based CHRP. “We hope funding a project that focuses on the issues facing transgender people will provide knowledge to help increase access to and uptake of PrEP in this population, and ultimately help to curtail the epidemic in this state.”
In these demonstration projects, PrEP will be delivered as part of a comprehensive prevention package, including risk reduction counseling, sexually transmitted infection screening and other components. Gilead Sciences, Inc. of Foster City, CA will provide the HIV prevention pill Truvada.
The three funded grantees are:
Team 1: University of California San Diego School of Medicine, Los Angeles LGBT Center and Family Health Centers of San Diego. Lead project investigators are Sheldon Morris, Robert Bolan and Christian Ramers, respectively. The team will also collaborate with University of Southern California and Harbor-UCLA Medical Center. Total 4-year budget: $3.75 million
These researchers will test if a transgender-focused case management approach to contextualize PrEP within the needs of the whole person can improve PrEP linkage and engagement in the transgender population. They plan to use an already developed personalized text messaging reminder system and will test if adding real-time counseling at times of missed doses will improve overall success in taking regular dosing over the course of study.
In addition, they will examine possible drug interactions between PrEP use and feminizing hormones by using the daily reporting of doses taken by text messaging to confirm whether the same drug levels expected to be protective for HIV are achieved by transgender women on hormonal therapy, and if taking PrEP is associated with any changes in hormone levels.
“This is truly an exciting opportunity to advance HIV prevention in transgender individuals with a high level of scientific rigor,” said principal investigator Sheldon Morris, MD, assistant professor of family medicine and public health at UC San Diego School of Medicine
Team 2: University of California, San Francisco (principal investigator Jae Sevelius and co-principal investigator Madeline Deutsch), The Gladstone Institutes (co-principal investigator Robert Grant), The Gender Health Center in Sacramento (co-investigator Ben Hudson) and La Clinica de la Raza in Oakland (co-investigator Leyla Welborn) Total 4-year budget: $2.9 Million
The team will develop and evaluate “Trans Research-Informed communities United in Mobilization for the Prevention of HIV (TRIUMPH)”, a culturally-relevant, community-led PrEP demonstration project driven by the needs and experiences of transgender women of color. The TRIUMPH uptake intervention consists of community-led mobilization efforts to increase knowledge and acceptability of PrEP, utilizing PrEP champions from within trans communities and trans-specific PrEP educational materials, including trans-specific patient decision aids that will assist people in making informed choices about PrEP.
To improve adherence, the team is planning an intervention consisting of peer-led health workshops and one-on-one personalized adherence counseling sessions. The team will also conduct a pharmacokinetic sub-study to investigate potential drug interactions between PrEP and hormone use. This research will answer important questions about how the proposed interventions affect people’s choices about whether or not to take PrEP, whether they take it as prescribed, whether PrEP is effective and whether participants take PrEP for the duration of the study.
“Our team has been conducting community-based research with trans communities across California and beyond for more than a decade, including behavioral HIV prevention intervention development for transgender women of color,” said Sevelius. “The HIV-related disparities experienced by trans women have been exacerbated by the ongoing aggregation of trans women with men-having-sex-with-men (MSM) data and the persistence of inadequate prevention approaches adapted from MSM strategies without knowledge or consideration of trans women’s unique sociocultural context. We believe these efforts will result in an unprecedented and highly valuable contribution to the field of HIV prevention among transgender communities.”
Team 3: San Francisco Department of Public Health Population Health Division (lead project investigators Albert Liu and Erin Wilson), Tom Waddell Urban Health Center (co-investigator Royce Lin), Castro Mission Health Center (Chris Nguyen), Asian Pacific Islander Wellness Center (co-investigator Tri Do) and Tri City Health Center in Fremont (co-investigator Zettie Page) Total 4-year budget: $2.6 Million
Team 3 will use a patient-centered medical home approach to develop and evaluate a comprehensive PrEP education, access and support package for HIV-negative transwomen and transmen in the San Francisco Bay Area (SFBA). The team will develop a broad, trans-specific social marketing campaign to increase knowledge about PrEP and will collaborate with staff to integrate PrEP delivery and support into four of the largest trans-specific clinics in the SFBA that provide culturally-competent care, including hormone provision. Specifically, their proposed interventions include a sexual risk assessment tool, online education, SMS-based adherence, reminders/support, panel management and peer navigators.
Research will determine the acceptability of the tools, PrEP uptake and adherence, most useful support strategies and measure any social harms and benefits of PrEP use. They will also investigate potential drug interactions between PrEP and hormone use. The long-term goal is to create a successful PrEP delivery and support model that can be scaled up to increase PrEP uptake and adherence among at-risk transgender women and men in California and the nation.
“These projects have the potential to fill an unmet scientific and public health need,” said Tri Do, MD, Chief Medical Officer at Asian & Pacific Islander Wellness Center. “More critically, the transgender community may finally get to see health care equity when it comes to new HIV infections.”
A feature-length article is available at californiaaidsresearch.org
Share This:
You May Also Like
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



