2019: A Space Organoid
UC San Diego researchers plan to send human brains-in-a-dish to the International Space Station to assess microgravity’s effect on neural development — and maybe prospects for life beyond Earth
Published Date
By:
- Jackie Carr
Share This:
Article Content
From the science fiction of Isaac Asimov and Arthur C. Clarke to the cinematic worlds of Star Wars and galaxies far, far away, humans have imagined life in space. But among the myriad challenges to colonizing other worlds lie fundamental questions of biology: Can a human embryo grow naturally outside the nurturing embrace of Earth? Will the brain form normally? How does weightlessness alter the basic, gravity-defined rules of human development?
A research team from University of California San Diego, led by Alysson R. Muotri, PhD, seeks to boldly go where the first answers may be found: Launching a payload of stem cell-derived human brain organoids to the International Space Station (ISS) orbiting almost 250 miles above Earth, where researchers will document how these masses of cells organize into the beginnings of a functional brain.
The first-ever project of its type is dedicated to T. Denny Sanford, a longtime advocate of stem cell research whose partnership has supported Muotri’s work as well as several key research entities, including the Sanford Consortium for Regenerative Medicine and UC San Diego Sanford Stem Cell Clinical Center.
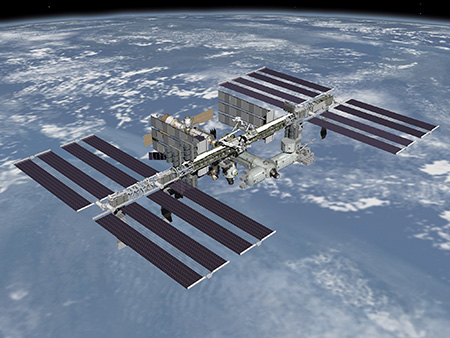
A research team from UC San Diego will launch a payload of stem cell-derived human brain organoids to the International Space Station to see if the cells develop normally in microgravity. Credit: NASA
“On July 21, UC San Diego will partner with Space Tango to launch a payload of living brain organoids into space,” said Erik Viirre, MD, PhD, professor of neurosciences and director of the Arthur C. Clarke Center for Human Imagination. “The study results will have enormous implications for space colonization and human health. We hope to determine if humanity can reach into the broader cosmos.”
“This groundbreaking experiment will evaluate more than 100 brain organoids, also known as ‘mini-brains,’ while in orbit,” said Muotri, professor in the UC San Diego School of Medicine Departments of Pediatrics and Cellular and Molecular Medicine. “We will be able to continuously observe the formation of the neural tube, including cell migration, cell-cell interaction, cell division and death. This will be the first in a series of space flights to help us understand the intricacies of brain development, both in weightlessness and on Earth.”
The mission, called BOARDS (Brain Organoid Advanced Research Developed in Space) has the NASA designation UCSD-ORG01 as a manifested payload on NASA’s Commercial Resupply Services cargo mission, SpaceX CRS-18. Space Tango, a developer of fully automated, remote-controlled systems for research and manufacturing on orbit, is designing the flight hardware to conduct the experiment in microgravity.
“This type of space experiment has never been done before for any type of stem cell-derived organoids. The engineering part of keeping these 3D structures alive in microgravity is a huge challenge,” Muotri said.
The brain organoids will travel inside a CubeLab, designed and built by Space Tango, that will be used to support continuous cell-culture during the mission. The CubeLab will be launched to the ISS in the SpaceX Dragon Capsule and installed in Space Tango’s TangoLab facilities onboard the ISS, providing remote, onboard monitoring of experimental data in near-real time.

The mission, called BOARDS (Brain Organoid Advanced Research Developed in Space), has the NASA designation UCSD-ORG01. Credit: Erik Jepsen, UC San Diego
After four weeks, the organoids will be returned to Earth for follow-up analysis, including molecular and cellular readouts, such as gene expression, epigenetics, morphology and metabolomics, which will be compared to Earth-based controls. In future space missions, the researchers hope to incorporate more sophisticated analyses, including dynamic electrophysiological recordings, which measure electrical activity and signals between cells.
“It’s been far too long that we’ve failed to grasp the importance of gravity in organ and embryonic development,” said David Brin, PhD, science fiction author, UC San Diego scholar-in-residence and advisor to NASA’s Innovative and Advanced Concepts program. “Our future path, in becoming an interplanetary species, could depend on discoveries that we’ll begin making with this mission.”
The researchers hope the brain organoids will also reveal molecular and cellular alterations that illuminate the biological processes of aging and disease states. If successful, the experiments will help scientists engineer new models to advance understanding of neurological disease and to generate novel treatments.
Global progress in the development of new treatments for neurological diseases has been challenging, in large part due to the lack of realistic experimental human models. Brain organoid models offer pharmaceutical researchers a way to advance research and development and the likelihood of approval of new treatments from Phase 1 clinical trials.
“Imagine if we could take a swab of cells from inside a patient’s cheek, revert the cells to stem cells, and then create a customized brain organoid for testing treatments,” said Viirre, also former chief medical officer for Zero G, a company that offers weightless flights. “With this model, derived directly from the patient, we can test thousands of different doses and medications and potential responses to treatment. This is personalized medicine at its best.”
Muotri said the dream is to one day use brain organoid models to pre-determine if a new treatment for autism spectrum disorder (ASD) or Alzheimer’s will be effective, before lengthy and expensive clinical trials.

The July 2019 flight to the ISS is dedicated to T. Denny Sanford by UC San Diego. Credit: UC San Diego
“This flight and future flights will help us create brain organoid models that will accelerate understanding of a range of neurological diseases,” said Muotri, who is also director of the UC San Diego Stem Cell Program and a member of the Sanford Consortium for Regenerative Medicine. “Ultimately, our findings may help shape future technologies and brain models to help scientists and doctors create more resilient brains.”
The Muotri lab has invented a new method to develop in vitro functional human brain organoids — three-dimensional, miniaturized, simplified versions of the organ produced from reprogrammed stem cells. Different from previous models, these brain organoids are able to display sophisticated neural network activity, with oscillatory brain waves similar to early stages of human neurodevelopment. The models have allowed Muotri and others to study biological functions with implications for better understanding ASD, Alzheimer’s and other neurological conditions.
Muotri is recognized as a leader in the field, having used the “brain-in-a-dish” approach to provide the first direct experimental proof that the Zika virus can cause severe birth defects, to repurpose drugs for a rare inherited neurological disorder and to genome-edit mini-brains to learn about human brain evolution.
Disclosure: Muotri is a co-founder and has equity interest in TISMOO, a company dedicated to genetic analysis and brain organoid modeling, focusing on therapeutic applications customized for autism spectrum disorder and other neurological disorders with genetic origins. The terms of this arrangement have been reviewed and approved by the University of California San Diego in accordance with its conflict of interest policies.
Share This:
Stay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



