Most of UC San Diego’s COVID-19 Cases Detected Early by Wastewater Screening
Part of the university’s Return to Learn program, wastewater screening helped prevent outbreaks by detecting 85 percent of cases early, allowing for timely testing, contact tracing and isolation
Published Date
By:
- Heather Buschman, PhD
Share This:
Article Content
People infected with SARS-CoV-2, the virus that causes COVID-19, are known to shed it in their stool, even if they aren’t experiencing any symptoms. With that in mind, University of California San Diego School of Medicine researchers have been screening wastewater from campus buildings for signs of the virus since the summer of 2020, thinking the information could help prevent outbreaks.
Now they have data to back it up: Screening for SARS-CoV-2 in wastewater, the team showed they can detect even a single infected, asymptomatic person living or working in a large building. Notification to occupants of each building with positive wastewater increased COVID-19 testing rates by as much as 13-fold. Once an occupant tested positive, isolation and contact tracing helped prevent further spread of the virus.
The approach enabled early detection of 85 percent of COVID-19 cases on the campus, researchers reported in the August 10, 2021 issue of mSystems. In other words, wastewater samples tested positive before most individual case diagnoses.
“University campuses especially benefit from wastewater surveillance as a means to avert COVID-19 outbreaks, as they’re full of largely asymptomatic populations, and are potential hot spots for transmission that necessitate frequent diagnostic testing,” said first author Smruthi Karthikeyan, PhD, an environmental engineer and postdoctoral researcher at UC San Diego School of Medicine.

Approximately 10,000 students lived on the UC San Diego campus during the 2020-2021 academic year, with low COVID-19 case rates thanks to the many risk mitigation, viral detection and intervention elements that make up the Return to Learn program. Credit: Erik Jepsen/UC San Diego.
Karthikeyan led the study with senior author Rob Knight, PhD, professor and director of the Center for Microbiome Innovation at UC San Diego.
Wastewater screening is an integral part of UC San Diego’s Return to Learn program, an evidence-based approach that has allowed the university to offer on-campus housing and in-person classes and research opportunities throughout most of the pandemic.
Return to Learn relies on three pillars: risk mitigation, viral detection and intervention. With approximately 10,000 students on campus during the 2020-2021 academic year, the many components of the program kept COVID-19 case rates much lower than the surrounding community and compared to most college campuses, maintaining a positivity rate of less than 1 percent during that time. The Return to Learn program, including wastewater testing, has become a model for other universities, K-12 school districts and regions.
Every morning, seven days a week, a team of students and staff in matching t-shirts deploys across campus on golf carts to collect sewage samples from 126 collection robots set up to monitor 350 buildings. By 10 a.m., they return to Knight’s lab at the School of Medicine.
There, Karthikeyan and team process the sewage using a different kind of robot, which concentrates the virus using magnetic nanoparticles, then extracts RNA — the genetic material that makes up the genomes of viruses like SARS-CoV-2 — from the samples. Polymerase chain reaction (PCR) testing is used to search for the virus’ signature genes.
When the virus is detected, automated but targeted messages are sent through a campus-wide system to persons associated with affected buildings, such as students, staff and faculty, recommending they be tested for the virus as soon as possible. The data is added to a public dashboard.
Since its inception, the team has worked constantly to optimize the process, Karthikeyan said. The current automated approach has dramatically reduced the sample-to-result turnaround time 20-fold; now five hours for 96 samples. By miniaturizing the samples, the researchers have reduced processing costs to $13 per sample. Knight estimates the approach exceeds the scale of similar surveillance programs by 10- to 100-fold. The next step, he said, will be to deploy rapid methods to test for SARS-CoV-2 variants, including delta, in real time.
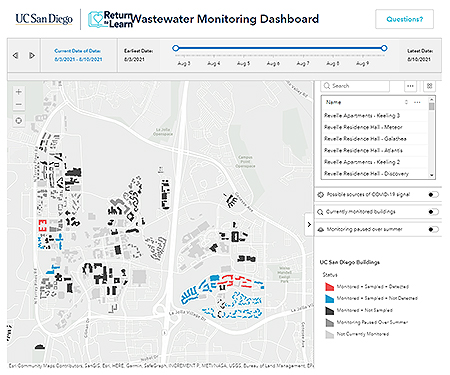
An online dashboard tracks COVID-positive wastewater detection on the UC San Diego campus and makes it available to the public. Credit: UC San Diego.
“This system demonstrates how the many different parts of UC San Diego can work together as a system to keep campus safe,” Knight said. “This work required not just advances in viral sample processing, but teams including Logistics, Environmental Health and Safety, campus and health system IT, Facilities Management, and many others, as well as leadership from the Return to Learn program to make it happen. We are now helping other campuses and organizations replicate this success, which has potential not just for COVID-19, but for many other stool-borne pathogens, including influenza, in future.”
Co-authors include: Andrew Nguyen, Daniel McDonald, Yijian Zong, Nancy Ronquillo, Junting Ren, Jingjing Zou, Sawyer Farmer, Greg Humphrey, Diana Henderson, Tara Javidi, Karen Messer, Cheryl Anderson, Robert Schooley, Natasha K. Martin, all at UC San Diego.
The research was funded by the UC San Diego Return to Learn program.
Share This:
You May Also Like
Engineers Take a Closer Look at How a Plant Virus Primes the Immune System to Fight Cancer
Technology & EngineeringStay in the Know
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.



